257x Filetype PDF File size 0.71 MB Source: www.mltj.online
ORIGINAL ARTICLE Nr 2020;10 (4):740-751
Lumbopelvic Stabilization Exercises and McKenzie
Method in Low Back Pain Due to Disc Protrusion:
A Blind Randomized Clinical Trial
1 2 2 2
M. B. Dohnert , C. Schwanck Borges , A. Steffen Evaldt , C. de Jesus Francisco ,
2 2 2 2 2
L. da Silva Dias , B. Chuaste Flores , G. Maciel Bello , R. Dimer da Luz , R. Boff Daitx
1
Research, Teaching and Extension Laboratory in Orthopedic Trauma Physiotherapy (LAPEFITO), Gurupi
University (UnirG), Gurupi, Torres, Brazil
2 Lutheran University of Brazil, Torres, Rio Grande do Sul, Brazil
CORRESPONDING AUTHOR: SUMMARY
Marcelo Baptiista Dohnert Introduction. Disc Protrusion (DP) is a degenerative spinal disorder. Lumbar interver-
Research, Teaching and Extension tebral disc protrusion is one of the most common orthopedic injuries, leading to low
Laboratory in Orthopedic Trauma back pain that radiates to the lower limbs. Physical exercise is the main element in the
Physiotherapy (LAPEFITO) conservative treatment of low back pain.
Objective. Comparing the effects of the McKenzie method and core stabilization exer
Department of Physiotherapy -
University of Gurupi - UnirG cises on the rehabilitation of patients with lumbar DP.
355 Joaquim Batista de Oliveira Street Methods. We allocated sixty-nine patients with low back pain due to disc protrusion
77.403-170 Vila Alagoana to the Core Group (CG), the McKenzie Group (MG), or the Core + McKenzie Group
Gurupi/TO, Brazil (CMG). All groups underwent three interventions per week for four weeks, totaling 12
E-mail: mdohnert@hotmail.com sessions. We assessed pain intensity, hamstring flexibility, functional capacity, muscle
strength, and lumbopelvic stability.
DOI: Results. All intervention groups significantly reduced pain intensity and functional
10.32098/mltj.04.2020.22 disability, besides improving posterior muscle chain flexibility, quality of life, trunk
muscle strength, and lumbopelvic stability (p < 0.05). For functional capacity, assessed
LEVEL OF EVIDENCE: 1B through the SF-26 Questionnaire, as well as for posture holding time in the lumbopel-
vic stability tests, the CG and CMG significantly improved the results compared to the
MG (p < 0.05).
Conclusions. The results suggest that both exercise methods were efficient in reducing
pain and improving function in patients with low back pain due to disc protrusion.
However, the groups that used stabilization exercises showed better results in activat-
ing lumbopelvic stabilizing muscles.
KEY WORDS
Low back pain; intervertebral disc displacement; physical therapy modalities; exercise
therapy; spine osteoarthritis.
INTRODUCTION (5, 6). Lumbar radiculopathy may be the result of a lumbar
Low back pain is a major health problem, with enormous disc protrusion or hernia that can irritate a sacral plexus
economic and social costs (1). Disc Protrusion (DP) is a trunk, leading to intraneural inflammation (6). A protrud-
degenerative spinal disorder (1). The degenerated disc has ing or herniated degenerated disc can cause paresthesia and
focal or localized abnormalities on the disc margin (2, 3). This weakness in the lower limbs, in addition to pain (6). In the
disorder relates to age, gender, prolonged workload, trauma, worst cases, lumbar radiculopathy can be chronic, resulting
and pregnancy (4). Lumbar intervertebral disc protrusion is in pain, disability, and substantial burden in the long run (6).
one of the most common orthopedic conditions, producing, This condition leads to health-related socioeconomic conse-
in many cases, low back pain that radiates to the lower limbs quences that directly affect well-being and quality of life (5, 7).
740
M. B. Dohnert, C. SChwanCk BorgeS, a. Steffen evalDt, et al.
Degenerated protruding discs and narrow spinal canals association, on the rehabilitation of patients with low back
are common conditions in the elderly (8). However, most pain due to disc protrusion.
subjects adapt perfectly well to the degenerative findings of
imaging tests, keeping in shape, and avoiding poor posture METHODS
(8). Physical activity is the main element in the prevention
and treatment of low back pain (9). It does not require Blind randomized clinical trial conducted from August
expensive materials, therefore providing an accessible inter- 2017 to June 2019. The study was registered in the Brazil-
vention in which the patient directly controls pain (9). ian Clinical Trials Registry (REBEC) under the identifica-
Spinal stabilization and the McKenzie approach are two tion number RBR-5mcvt6. The study was approved by the
different interventions for the treatment and preven- Committee of Ethics on Human Research of Universidade
tion of low back pain (9). The core stabilization program Luterana do Brasil under the number 2, 152, 592 (21).
emphasizes the training of specific deep or local stabiliz-
ing muscles of the spine, keeping the lumbar region in a
neutral position during occupational and daily life activities Sample calculation
(10). The McKenzie method, also called Mechanical Diag- We used pain intensity, measured by VAS, as the primary
nosis and Therapy (MDT) (8), emphasizes an examination/ outcome of the study. Based on the study by Hasanpour-De-
treatment that incorporates repeated spinal movements hkordi, Dehghani and Solati (11), we used a study power of
(10, 11). The patient’s response to these repeated move- 80%, a 95% Confidence Interval, and a sample size ratio
ments determines a classification and a preferred direc- of 1:1:1 (Core; McKenzie; Core + McKenzie) to estimate
tion for therapeutic exercise (11-14). Postural correction the number of participants for each intervention group.
and maintenance of normal lordosis are an integral part of Believing that losses and refusals would be around 20%, we
the McKenzie program, and treatment programs general- reached the final number of 23 participants for each study
ly emphasize the performance of repeated lumbar move- group, totaling 69 participants.
ments for the effective management of specific syndromes
(13). This method considers the patient’s symptomatic and
mechanical response to repeated movements and sustained Sample randomization
postures for evaluation and treatment (8, 14). Therefore, After the initial assessment, we randomized the eligible
it uses a directional preference to reduce or increase the participants by using a list of random numbers provided by
®
patient’s symptoms (12, 14). the EPI-Info software. We allocated a total of 69 patients
The spinal stabilization system, also called core system, to the following groups: McKenzie Group (MG), which
is composed of the spinal column, which provides intrin- performed only one McKenzie exercise protocol, Core
sic stability, muscles that provide dynamic stability, and a Group (CG), to which we applied lumbopelvic stabiliza-
neural control unit that evaluates and determines the stabil- tion exercises, and Core + McKenzie Group (CMG), which
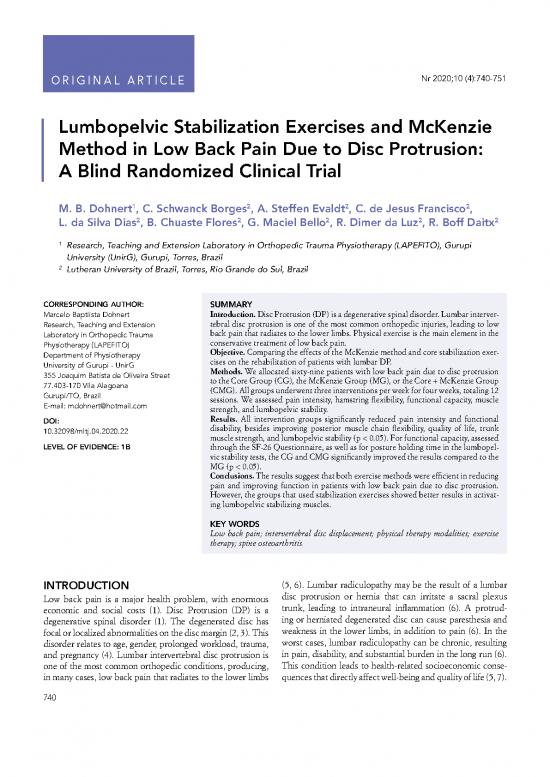
ity and coordination requirements of the muscle response performed both protocols (figure 1).
(8). The central stabilizing muscles, also called core muscles,
are categorized, according to their function, as glob-
al muscles (rectus abdominis, spinal erectors, and external Elegibility criteria
obliquus abdominis) and local muscles (transversus abdomi- The study included 69 patients of both genders, aged
nis and lumbar multifidus) (15). Global muscles participate between 18 and 65 years, who had low back pain due to
in trunk movements, while local muscles play an important disc protrusion. The participants should have complemen-
role in stabilizing the core (15). The transversus abdominis tary exams (magnetic resonance or computed tomogra-
and the lumbar multifidus play important roles in the func- phy) showing DP and/or herniated disc, and should not be
tional activities of the spine (15). Core stabilization exercis- performing any other type of physiotherapeutic approach
es aim to activate central muscles, including the transversus for low back pain at the time of the study. All participants
abdominis, lumbar multifidus, and paraspinal, abdominal, signed the Informed Consent Form (ICF).
diaphragmatic, and pelvic muscles. This provides spinal We excluded from the study patients who had severe spinal
stability and prevents lumbopelvic injuries by controlling pathologies (fractures, tumors, and inflammatory pathol-
joint tension, strengthening muscles, increasing resistance, ogies such as ankylosing spondylitis), who had previous-
and correcting posture (7, 16-20). ly undergone lumbar surgery, patients with severe cardio-
The present study compares the effects of the McKenzie vascular and cardiorespiratory disease, pregnant women,
method and core stabilization exercises, as well as their patients who did not attend three consecutive or intermit-
Muscles, Ligaments and Tendons Journal 2020;10 (4)
741
Core Exercises and McKenzie Method in Lumbar Disc Protrusion
Recruited for the
study (N=104)
Excluded (n=18)
Age over 65 years (n=2)
Referral for surgery (n=2)
No schedule availability (n=5)
Without MRI or CT examination (n=8)
Performing another type of physical
therapy approach (n=1)
Randomised
(N=86)
Allocated to the Allocated to the
MG (N=31) CMG (N=28)
Allocated to the
CG (N=27)
Interrupted Interrupted
intervention (n=8) intervention (n=5)
* Withdrawal Interrupted * Withdrawal
intervention (n=4)
* Withdrawal
Analyzed (N=23) Analyzed (N=23) Analyzed (N=23)
Figure 1. Flowchart – Recruitment and evaluation of patients with disc protrusion.
RM: MRI; CT: Computed Tomography; CG: Core Group; MG: McKenzie Group; CMG: Core + McKenzie Group.
tent consultations, and those that presented some neuro- Pain intensity assessment
logical disorder that prevented them from performing the We assessed pain intensity by using the Visual Analogue
proposed exercises. Scale (VAS). In this scale, the evaluator asks the patient
about his/her pain level on a scale from zero to ten, where
zero means total absence of pain and ten the maximum
Data collection tolerable pain.
The evaluation protocol was conducted by a blind evalua-
tor, that is who did not know which group the participant Quality of life assessment
belonged to. The evaluation took place in two stages of the We assessed quality of life by using the SF-36 Question-
study: initially – prior to the randomization of the subjects, naire. This instrument consists of 11 questions and 36 items
and at the end of the intervention protocol. that encompass eight domains represented by functional
capacity, physical aspects, pain, general health status, vital-
Anthropometric assessment ity, social aspects, emotional aspects, and mental health.
We calculated the Body Mass Index (BMI) by measuring The application of this questionnaire takes place through
body height and weight. the attribution of a score for each question, later trans-
Muscles, Ligaments and Tendons Journal 2020;10 (4)
742
M. B. Dohnert, C. SChwanCk BorgeS, a. Steffen evalDt, et al.
formed into a scale from “0” to “100” per domain, where Lumbopelvic stability assessment
“0” corresponds to the worst quality of life and “100” the To analyze lumbopelvic stability, we applied the Single Leg
best quality of life. Squat Test (unilateral squat), the Runner Pose Test, the
Prone Instability Test, the Right and Left Lateral Bridge
Functional capacity assessment Test, and the Sorenson Test (extensor endurance test).
To quantify disability, we used the Roland-Morris Disabili-
ty Questionnaire. This instrument consists of 24 items that
describe daily tasks that patients have difficulty performing Intervention protocol
due to low back pain. The questions have a dichotomous The intervention protocol consisted of three interventions
answer (yes or no), and the result corresponds to the sum per week for four weeks, with all study groups performing
of the yes answers. This result can vary between 0 and 24, a total of 12 sessions. The service took place individually.
with zero corresponding to a person without complaints, Each session lasted between 40 and 60 minutes. Initial-
and the maximum value corresponding to a patient with ly, all participants performed a 10-minute stationary bicy-
very severe limitations. The greater the number of alterna- cle warm-up. Afterwards, we performed the intervention
tives filled in, the greater the functional impairment. We according to the randomized group. The intervention proto-
instructed the individuals to complete the items that better col was applied by a researcher previously trained and famil-
described them on the day of application. iar with the protocol. The interventor controlled during the
sessions the technique of performing each exercise, as well
Hamstring flexibility assessment as its intensity and duration in both intervention groups.
We measured hamstring flexibility by using the Wells bench.
For performing this test, the patient seated with legs extend- Intervention protocol for the McKenzie Group
ed and feet supported on the device. Then, the individual The intervention protocol for the MG consisted of three
should flex his/her trunk and hips the maximum possible, sets of exercises with 10 repetitions each, with a 30-second
with hands superimposed and supported on the measuring interval between sets. We maintained the exercises for five
tape installed on the upper part of the Wells bench. The seconds initially, subsequently maintaining them for 10
evaluator asked the patient to stretch his/her hands as far as seconds according to the patient’s performance. We defined
he/she could reach without bending the knees, thus obtain- the treatment from the result of the evaluation performed
ing the maximum reach point. prior to the randomization stage, and guided it according to
the preferred direction of movement, that is flexion, exten-
Trunk extensor muscle strength assessment sion, or lateral displacement of the spine. We applied the
We assessed trunk extensor muscle strength by using McKenzie protocol according to Garcia et al. (13) (table I).
®
the Crown dorsal dynamometer. In this test, the patient
remained standing, with feet supported and parallel, knees Intervention protocol for the Core Group
extended, and the spine initially flexed. At the command In the CG protocol, we developed the exercises accord-
of the examiner, the patient extended the spine by holding ing to the studies of Moon et al. (21), who used eight exer-
the lever bar with his/her upper limbs for dynamometer cises based on static postures, initially maintained for five
measurement. seconds. As the program evolved, the degree of difficulty
Table I. McKenzie group exercise protocol.
Exercise Number of repetitions
Exercise 1. Flexion of the lower limbs on the bench press 3 sets with 10 repetitions
Exercise 2. Bending the trunk while sitting on the chair 3 sets with 10 repetitions
Exercise 3. Standing trunk flexion 3 sets with 10 repetitions
Exercise 4. Prone trunk extension 3 sets with 10 repetitions
Exercise 5. Standing trunk extension 3 sets with 10 repetitions
Exercise 6. Lateralization of the standing pelvis 3 sets with 10 repetitions for each side
Exercise 7. Lateralization of the pelvis against the wall 3 sets with 10 repetitions for each side
Muscles, Ligaments and Tendons Journal 2020;10 (4)
743
no reviews yet
Please Login to review.