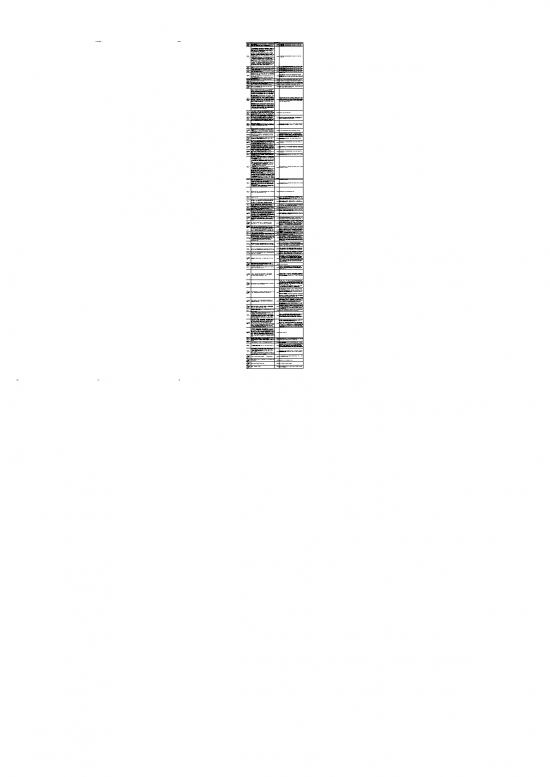
269x Filetype XLSX File size 0.08 MB Source: www.michigan.gov
Sheet 1: SCA Q&A
| State of Michigan, Department of Health and Human Services | ||||
| Standard Cost Allocation Methodology | ||||
| SCA Q&A Tracking | ||||
| No. | Agenda Topic | Issue/Question | Q&A Release Date | Response and/or Proposed Changes |
| 1 | Allocation Clarifications | May require not to change things, so requires 'actuals' based on FTE. Will need to be consistent across the organization. | 4/23/2021 | This has been addressed in the methodology report released in April 2021. SCA Workgroup discussed on 1/29/21 |
| 2 | Allocation Clarifications | So you would have to go back and adjust what you had allocated based upon FTE? It may require you to not go back and change things – so it would have to be based on actuals |
4/23/2021 | This has been addressed in the methodology report released in April 2021. SCA Workgroup discussed on 1/29/21 |
| 3 | Allocation Clarifications | I want to share my concerns with the workgroup about allocating employee insurance expense by FTE as proposed by the draft version of the PIHP and CMHSP Standard Cost Allocation Methodology. Paragraph 6.6.1 of the GF contract states “The CMHSP will comply with generally accepted accounting principles (GAAP) for governmental units when preparing financial statements. The CMHSP will use the principles and standards of 2 CFR 200 Subpart E Cost Principles for determining all costs reported on the financial status report…” 2 CFR 200.431 (d) specifically defines 2 methods of allocating fringe benefits. 2 CFR 200.431 (d) states “Fringe benefits may be assigned to cost objectives by identifying specific benefits to specific individual employees or by allocating on the basis of entity-wide salaries and wages of the employees receiving the benefits. When the allocation method is used, separate allocations must be made to selective groupings of employees, unless the non-Federal entity demonstrates that costs in relationship to salaries and wages do not differ significantly for different groups of employees.” As shown above, either 1) specific benefits to specific employees or 2) allocating on the salaries and wages of the employees receiving the benefits is considered allowable by 2 CFR 200. Using FTE to allocate employee insurance expense would be inconsistent with the fringe benefit allocation methods prescribed by 200.431 (d). Option 2) is a viable method of allocating fringes benefits and does not require allocating at the individual level. In fact, option 2) already appears to be used into the Standard Cost Allocation Methodology to allocate pension and retirement expenses. It is my understanding that the Standard Cost Allocation Methodology will be used to produce to the Financial Status Report (FSR) and per the Contract paragraph 6.6.1, the FSR needs to follow 2 CFR 200 Subpart E. Furthermore, federal grant expenditures need to be allocated in accordance with 2 CFR 200 and deviations from the cost principles described in 2 CFR 200 may result in questioned costs during a single audit. I would encourage the workgroup to consider Option 2 noted above as an viable alternative to allocating fringe benefits by FTE. |
4/23/2021 | This has been addressed in the methodology report released in April 2021. SCA Workgroup discussed on 1/29/21 |
| 4 | Allocation Clarifications | Can specific Other Expenses be allocated on some basis to multiple cost centers rather directly assigned? | 4/23/2021 | Items such as Room and Board, cannot be allocated, which is why it is set as directly assigned. Other items (e.g. mailroom expenses) identified as Other Expenses can be directly assigned to General Administration or IT. |
| 5 | Allocation Clarifications | Need to discuss whether Other Expense should be allocated and we need either a specified Room & Board expense category OR we have two Other Expense categories (one that is directly assigned and another that is allocated). | 4/23/2021 | Items such as Room and Board, cannot be allocated, which is why it is set as directly assigned. Other items (e.g. mailroom expenses) identified as Other Expenses can be directly assigned to General Administration or IT. |
| 6 | Allocation Clarifications | Can specific other expenses be allocated on some basis to multiple cost centers rather directly assigned (such as telephone office supplies)? | 4/23/2021 | Items such as Room and Board, cannot be allocated, which is why it is set as directly assigned. Other items (e.g. mailroom expenses) identified as Other Expenses can be directly assigned to General Administration or IT. |
| 7 | Allocation Clarifications | I have a question specific to our CMHSP. We are still a department of our County, and therefore we are charged as part of our County Cost Allocation Plan for things such as space, maintenance, most of the IT costs, HR, payroll, etc. This typically is recorded in one expense account and then we are spreading this across all cost centers based on the FTE count. Could you please take into consideration how we should handle this as it pertains to the new allocation template and logic? |
4/23/2021 | This expense can be identified as an Other Expense and can be directly assigned to General Administration or IT. Ideally, amounts allocated from the county could be separately identified as facility related, IT related, and all other functions. There will be some cases where the SCA Workgroup will need to provide TA to certain CMHSPs. |
| 8 | Managed Care Administration | Need to review the IT costs to determine if there is a more appropriate way to get claims processing separate from other IT | 4/23/2021 | Claims processing is being included within Other Managed Care Administration and is separate from IT |
| 9 | Expense category strategy | Where would compensated absences liability be reported? | 4/23/2021 | This is a balance sheet item, but the expense is likely part of salaries/wages for the employee. |
| 10 | Allocation Clarifications | This will impact grants/contracts that will not allow us to go back to the beginning of the year to adjust the insurance/pension allocations that have been billed to them. | 4/23/2021 | Estimate as best possible and at year end do cost adjustments, but this is not applicable for this year. |
| 11 | Allocation Clarifications | MH courts contracts require actual not estimate, no allocation, based on employee and required documentation. In that case, it would be direct allocation and create a mixed approach. | 4/23/2021 | This has been addressed in the methodology report. SCA Workgroup discussed on 1/29/21 |
| 12 | Non-Encounterable cost center clarifications / changes | Recipient Rights - Are Recipient Rights Trainings considered trainings from the Training Department or part of the Recipient Rights cost? | 4/23/2021 | Recipient rights costs include the cost of the trainers. The 2 hours for individuals attending training should still be charged to their direct service cost center. |
| 13 | Non-fee for service contracts/Reporting network provider costs | In the Cost Allocation training #1, the comment was made that CMH/PIHP should be able to pull the encounter data to report cost. In our current processes, we do add up the total from encounters but always need to do some adjustment to match the amount we have actually paid to providers because of some of the non-Fee for Service contracts that we have with Providers. In those contracts we have estimated the number of encounters and costs. Examples of non-Fee for Service contracts would be Daily or Monthly case rates, Net Cost Contracts, and Value Based Purchasing arrangements. Below are examples of those types of contracts and how we establish the encounter rate. How would these examples would play out in the Cost Allocation process? Daily/Monthly Case Rate: For ACT services, we pay the outside provider a per day amount for each enrolled ACT Consumer provided they have documented contact with that Consumer during the month. We use a CPT code for the actual billing that does not get submitted to the PIHP and also require the Provider to submit encounters with the actual CPT code. The Actual CPT code does submitted to the CMH does not include a charge amount. At the CMH level, we have calculated the cost per encounter based on expected billable (productivity) amounts. Let’s say the rate was based on providing an average of 12 ACT units per month per consumer. However the actual average units per month per person are 6. Thus the actual cost to provide that service is double the amount that we have calculated and reported throughout the year. In order to report the appropriate costs for ACT services , would we need to pull all those encounters back at the end of the year, re-price them and then resubmit them or is there another option? Net Cost contracts We have several net cost contracts with Providers where we cover the entire cost of the program based on an annual budget they submitted. They do submit encounters for billable services that have a zero charge. As in the example of daily/monthly case rate, we have calculated the charge amount that gets applied to the encounter before it is sent to the PIHP. So, lets say the encounter rate based on previous year encounters and total program cost is $100.00 per unit. However during the current year, they do not incur the same amount of costs and they provide more billable units than anticipated. In order to report appropriate costs, would those encounters need to be pulled back at the end of the year, re-priced , and then resubmit with a changed charge amount that would more closely reflect the total amount paid to the provider. |
4/23/2021 | For non-FFS contracts with network providers, the Service UNC tab should reflect what is included within the encounter data (i.e. so that entities can summarize their data warehouse to populate). A separate tab in the EQI template will be created to capture all adjustments to expenditures for non-FFS contract arrangements, including documentation of the contract type, the information included in encounters, and the actual expenditures incurred. There will be a separate row for each provider and procedure code. CMHSPs will need to begin collecting start/stop times for contracted services to support this reporting beginning 10/1/2022. |
| 14 | Non-fee for service contracts/Reporting network provider costs | –“ Note that there will be instances where services are provided through contractual arrangements with network providers that “bundle” services together, or are provided under sub-capitated contractual arrangements. In these instances, network provider contracts will require modification to require that network providers can report actual services and related payments for the services at the individual service level.”, Page 18 item 6 Does this suggest that all Provider Contracts need to be Fee for Services based? If not, how would a Net cost type contract comply with this requirement? | 4/23/2021 | See above. FFS contracting is not a requirement. |
| 15 | Non-fee for service contracts/Reporting network provider costs | Medical Loss Ratio - Incurred claims: direct claims paid to providers (including under capitated contracts) for services covered under the contract, unpaid claims liabilities, provider withholds and incentive/bonus payments, and claim payments recovered from fraud reduction efforts (not to exceed the amount of fraud reduction expenses which must not include fraud B29prevention activities). Non-claims costs must be excluded with the exception of administrative costs attributable to direct provision of Medicaid covered services by CMSHP provider employees, which may be included with incurred claims.23 I believe the statement was also made that the Network Provider claims should be able to be pulled directly from the encounters. How would unpaid claims liabilities and incentive/bonus payments be included in Provider Network payments? | 4/23/2021 | Unpaid claim liabilities, incentives, and bonuses paid to providers should not be included in the encounter data and can be reported on the Other Expense tab of the EQI template. These expenditures should be included in incurred claims of the MLR. |
| 16 | Non-fee for service contracts/Reporting network provider costs | Value Based Contract (incentive pay) If we have a contract with a provider to give a performance bonus amount if certain measures are met, do those costs need to be reflected in the encounters or would those performance payment amounts not be included in the MLR calculation? If not in the MLR (or incorporated into the cost of providing the unit) would they be Managed Care Administration costs? |
4/23/2021 | Incentives and bonuses paid to providers should not be included in the encounter data and can be reported on the Other Expense tab of the EQI template (row 13). These expenditures should be included in incurred claims of the MLR. |
| 17 | Assignment of Salaries and Wages | a. We contract with Psychiatrists by the hour and they provide services in person at our office or via telepsych, We provide MA staff, space, receptionist and IT. How do we split this between contractual and cover the support costs that we provide? We use their NPI number to bill. Yes as billing provider. b. Psychiatrist is contractual staff (03 category), compensation directly assigned to cost center (or multiple) based on the work. Support staff goes to the cost center and IT is allocated based on methodology. Workgroup further discussion. |
4/23/2021 | James followed up and indicated they do use the CMHSP billing provider NPI in this example. |
| 18 | Managed Care Administration | Earlier you showed Access including benefit eligibility activity and MPM shows targeted case management assisting the beneficiary to access programs that provide financial assistance. Discuss the difference please. | 4/23/2021 | Allocation to encounterable/clinical services should occur first in alignment with the Michigan Medicaid Provider Manual and Mental Health Code Sets documentation. Access activities as documented in MDHHS' policy "Access Standards" should be assigned to the non-encounterable cost center "Access Center" which is then allocated to the administrative cost category "Shared managed care administration." Provider front office activities to verify eligibility at the point of care are not considered access and instead should be reported as "General Administration." |
| 19 | Non-Encounterable cost center clarifications / changes | CMHSP must get into a contractual relationship with the FI. What am I supposed to do with this in the cost allocation; Incurred claims will be what is paid to the provider; The administration associated with the Self-Determination – where does it go? |
4/23/2021 | We have added Self-Determination Administration as a non-encounterable cost center so this is separately identifiable |
| 20 | Assignment of Salaries and Wages | I am struggling just a bit on collection of costs of certain areas. Example would be behavior treatment. That is a team of different credentialed staff and supervisors collected under different cost centers. H2000 is a team based services with staff under different clinical cost centers. Those staff would need to be allocated across appropriate costs centers. Also true of administrative costs. Key task to get salaries and wages where services are being provided. Will have additional discussion on the best way to allocate across cost centers. | 4/23/2021 | Additional training will be provided detailing approaches for assigning salaries and wages across multiple cost centers |
| 21 | Assignment of Salaries and Wages | Hi – the response provided to the concern of how to allocate minutes to the H2000 was to be sure to have payroll costs in the appropriate cost centers for the members of the team, however this code is entered by one staff participating in the treatment team meeting. How would we allocate the complete cost of the team to the service if the service will come in with the modifier of the staff that enter the service. Currently our Behavior Treatment Committee chair enters the service for each of the cases that are reviewed during the monthly meeting. A cost per meeting is calculated by summing the cost of the team members. The total annual cost is spread to the number of units for the year. Can you explain how this could then be put into the template? | 4/23/2021 | Salaries and wages for all staff involved in the behavior treatment plan should be allocated to the behavior treatment cost center. This is a team-based service and would not include a provider group modifier. |
| 22 | Assignment of Salaries and Wages | Our psychiatrists will provide ABA assessment or identification as well as medication Administration. What is the thought on assigning a cost center? Option 1 - encounter would show minutes on each activity and directly allocate based on service provided. Option 2 - documentation of time on each activity and then allocate to the cost centers. |
4/23/2021 | Additional training will be provided detailing approaches for assigning salaries and wages across multiple cost centers |
| 23 | Service Cost Centers | My understanding is that treatment planning is one of the activities included in case management services, meaning that T1016 or T1017 would be coded. If so, why would H0032 be included as a case management service? Wouldn't it be more appropriate to include H0032 under outpatient? Workgroup agreed to look at again. | 4/23/2021 | We have updated the cost centers for each procedure code to include variation for different provider groups performing the same service. |
| 24 | Service Cost Centers | Would the workgroup re-visit the placement of H0032 (treatment planning) in the Case Management cost center (as indicated in Appendix 2)? There is language in the PIHP/CMHSP Encounter Reporting HIPCS and Revenue codes document that would seem to conflict with this placement. The language excerpts below would seem to indicate that H0032 should be in many cost centers, but not in case management as Case managers and/or supports coordinators do not report treatment planning. i. H0032 - When/how to report encounter: 1. -Count independent facilitator and all professional staff, where the consumer has chosen them to attend, participating in a person-centered planning or plan review session with the consumer 2. -Case manager or supports coordinator do not report treatment planning as this is part of TCM and SC 3. -Report monitoring the implementation of part(s) of the plan by clinician, such as OT, PT or dietitian. 4. -Assessments and evaluations by clinicians should not be coded as Treatment Planning but rather as the appropriate discipline (e.g., OT, PT, speech and language) 5. -Use Modifier TS when clinician performs monitoring of plan face-to-face with consumer 6. Allocating and reporting costs 7. -Major implications for indirect contribution to other activities 8. -Indirect activity 9. -The cost of a clinician’s monitoring the implementation of plan that does not involve a face-to-face contact with the consumer is an indirect cost of treatment planning ii. Other ambulatory/outpatient services that can be reported at same time iii. Treatment Planning (H0032) can be reported by an independent facilitator and all professional staff for the same session. In addition, it can be reported by multiple staff at same time that the case manager/supports coordinator also reports that time using their own code: T1016, T1017, H0039, H0036, H2022, or H2021. It should be noted that only one staff person can attend an IPOS in the behavioral health case management role. In their role providing services and supports planning, Adult Peer Specialists and Recovery Coaches will report H0032 with their appropriate, respective modifiers. Youth Peer Support Specialists will report H0038 with the TJ modifier and Parent Support Partners S5111 with the HM modifier. iv. 11. Face-to-face interactive Case Management monitoring (T1016/T1017) can be reported at the same time as in-home service such as community living support and personal care, and certain day-time activity services (clubhouse, supported employment, prevocational service, skill building, community activities). Professionals and specialty providers will report treatment plan monitoring (H0032-TS) at the same time that the consumer is receiving the service for which they are being monitored in the above settings. v. 12. Face-to Face monitoring by home-based staff (H0036) and ACT (H0039) team members can be reported at the same time as day-time activity services. The consumer must be present and have at least 15 minutes of interaction with the home-based staff or ACT team member for the monitoring activity and the service being monitored to be reported at same time. |
4/23/2021 | We have updated the cost centers for each procedure code to include variation for different provider groups performing the same service. |
| 25 | Service Cost Centers | Additionally, would the workgroup include treatment planning monitoring (H0032:TS) to determine which costs centers that code could be used in? | 4/23/2021 | We have updated the cost centers for each procedure code to include variation for different provider groups performing the same service. |
| 26 | Service Cost Centers | The chart seems to imply that codes with modifiers would follow in the same cost centers as the primary code (without the modifier) . However, there are a few codes where the modifier may need to be placed differently from the main CPT code. Below are two examples: 1. Behavior Treatment – The Behavior treatment monitoring code does not seem to be included in the codes (H2000:TS) for any of the programs listed. I am not sure it belongs in BT. For our organization, this code is reported in the IDDA Supports Coordination/case management and provided by the Psychologist. Several of our Residential contracts also allow for BT monitoring. Where would this code belong? 2. Case Management – The code for Treatment Planning (H0032) is included in the Case Management cost center. It does not appear that the Treatment Plan Monitoring code (H0032:TS) is identified in any of the cost centers. Where does this code belong? |
4/23/2021 | We have updated the cost centers for each procedure code to include variation for different provider groups performing the same service. |
| 27 | Service Cost Centers | Health homes need cost centers. Does there need to be separate cost centers for the health home service costs separate from the health home administrative costs? | 4/23/2021 | We have added a cost center for the health home procedure codes. |
| 28 | Service Cost Centers | Where do CCBHC costs go? | 4/23/2021 | CCBHC costs will not be treated differently than any other costs incurred by CMHSPs. These additional costs should be identified in the most appropriate cost center. We will make adjustments to be explicit about excluding all of the non-allowable costs shown in the CMS CCBHC cost report from the clinical and non-encounterable cost centers. |
| 29 | Service Cost Centers | In Appendix 2, the S9484 code is the only code listed for the Crisis/mobile Crisis cost center, see below: 109 Crisis/Mobile Crisis S9484 It is our understanding that an Intensive Crisis Response team can also use the following: Intensive Crisis Stabilization S9484, H2011 TJ, H2011 HB, H2011 HC, H2011: Below are excerpts from the guidance: Crisis intervention mental health services, per hour. Use for the - MDHHS-approved program only. PLEASE NOTE EFFECTIVE 10/1/18: S9484 TJ – will no longer be used for ICSS for children, because the 1-hour time requirement does not accurately reflect the services being provided. MUST USE H2011 TJ for Children. PLEASE NOTE EFFECTIVE 10/1/18: ICSS for Adults CAN use the H2011 HB or H2011 HC to report if they do not meet the one hour minimum OR use the S9484 if meets the one hour requirement for this code. CAN USE H2011 or S9484 for Adults. Hour DT=24/day H2011 - this service must be initially reported at 30 minutes and in 15-minute increments thereafter. DT: H2011=96/day Line Professional State Plan, Healthy Michigan, EPSDT When/how to report encounter: Face-to-face contacts only, other contacts (phone, travel) are incorporated in as an indirect activity Allocating and reporting costs -Costs of the team -Bundled activity -Cost and contact/productivity model assumptions used -Account for contacts where more than one staff are involved Please review and determine if the codes for Cost Center 109 should be updated. |
4/23/2021 | We have discussed this issue with MDHHS and will be utilizing H2011 HT to identify Mobile Crisis services for children and adults. MDHHS will be developing guidance regarding the requirements to be considered a qualifying Mobile Crisis team. |
| 30 | Service Cost Centers | Definition of Care Coordination includes Person-centered planning process and self-determination. Does the Person centered planning process include the non -encounterable time of a Independent Facilitator when working on the development of the Person Centered Plan (this is separate from the IPOS) ? | 4/23/2021 | The independent facilitator is by rule a contracted network provider and should be included within the direct-run cost centers. The non-encounterable time of the independent facilitator should be added to the cost of the service (H0032) a CMHSP pays a network provider to deliver. |
| 31 | Service Cost Centers | Outpatient – includes 90792, which is a psych eval with Med Monitoring. No other Psych codes are included in the Outpatient program. It would seem that Psychiatric Services – Med clinic would be a better fit for that code. Can this code be moved to Psychiatric Services? | 4/23/2021 | We have updated the cost centers for each procedure code to include variation for different provider groups performing the same service. |
| 32 | Managed Care Administration | The costs within 05 are a mix of provider administration and subcontractor/managed care administration costs. They need to be separated. | 4/23/2021 | The group has discussed the separating these items would require significantly more detail in time tracking for staff and have opted to move forward with what is currently proposed for the initial SCA methodology. If needed, this could be updated in future years. |
| 33 | Assignment of Salaries and Wages | In the Rate Setting workgroup, there were some salary and wages that were directly included in the cost of the service. For example, 90792 Psych assessment included 90 minutes of Nursing time. Since these individuals provide direct support for this services, It is appropriate to include Nursing/ MA costs (directly as part of the rate) into the services provided in a Psychiatric Med clinic. Would the salaries and benefits of RN/ MA’s be considered Salary and Wages – Clinical direct service staff for all the Evaluation and Management codes? Should the salary and wages of individuals who are included in the rate development template (s) as being directly involved in the encounter, be included in the Salaries and Wages -clinical direct service staff line? | 4/23/2021 | We agree that these clinical staff should be included within the expense category line Salaries and Wages - Clinical direct service staff. Individuals included within the independent rate model would be included in this expense category for those services. |
| 34 | Assignment of Salaries and Wages | Our Psych Med clinic program includes support staff that check in/out Consumers and nursing triage services that are mostly non-billable phone contacts. Currently these costs are included in the cost of the services provided by the Doctors and Nurses in that clinic. If I understand the new model, those salary dollars would be included in an admin cost center and spread across all programs even though those individual support staff only provide services to the Psych clinic. Is that accurate? | 4/23/2021 | We have added a separate expense category for service support staff salaries and wages so that their costs can be identifiable and directly assignable into direct-run cost centers. This would still be considered provider administration for purposes of the independent rate model comparison. |
| 35 | Non-Encounterable cost center clarifications / changes | What is the definition of second-line supervision? If I remember correctly, the rate setting templates only include the first line supervisor. Should these structures be in alignment? | 4/23/2021 | Supervision Definition: Time and expenses for first- and second- line supervisors in the oversight and management of directly reporting clinical staff. As with clinical staff, first- and second-line supervisors are also on-site and client facing, although their supervisory time does not result in a billable service. In addition to providing direct oversight of clinical staff, supervisory staff are those primarily responsible for supervising, hiring, and training the clinical staff that actually provide the billable services. Supervisor responsibilities may also include program planning and evaluation, advocacy, working with families, performance management and discipline, and working with community members. |
| 36 | Assignment of Salaries and Wages | I had a question in regards to the attached Appendix 3 spreadsheet. Will we be required to separate salaries based on education level in our payroll system and cost allocation worksheet? | 4/23/2021 | No, that detail is not required in payroll systems or cost allocation; it is only required in the encounter data |
| 37 | General | Is there a plan to require the SCA workbook to be submitted as part of the annual required reports? Will we be expected to use the tool to actually allocate our various expenses such as support staff, supervisors, building expense, IS, auto & etc.? Or will it be ok to allocate these expenses in our accounting software as long as we use the required method such as square feet or FTEs? | 4/23/2021 | The intent is to require components of the SCA Model as part of annually required reporting (e.g., Final DRClinical CC Summ tab). There will be some flexibility in model use so long as the allocation methodology is followed (e.g., facilities allocated by square footage in the general ledger would be allowable and the model can accommodate that). There may be some expenses deemed to be immaterial that would not be required to have a consistent allocation methodology (e.g., workers compensation). |
| 38 | General | When will the final SCA model/workbook be complete? | 4/23/2021 | A Revised Draft model will be provided following the April training. Additional models will be provided as needed in the future based on additional feedback from the field. |
| 39 | General | Will there be another training after we’ve had additional time to work through the new cost centers, standard expense categories and etc. to review how costs are allocated using the model? And to answer additional questions that I’m sure will arise? | 4/23/2021 | The intent is to have bi-weekly FAQ sessions during which CMHSPs can ask additional questions that will arise during implementation of the new SCA model |
| 40 | Managed Care Administration | Managed care or delegated administration: my view is that all of the CMH for Central Michigan’s administration is related to direct or contracted services and other non-encounterable costs. All of the agency’s administration expense would be incurred if we were a standalone provider of service – if we didn’t have a PIHP all of our administration costs would be incurred. Because of this it is difficult to determine what percent of admin time is managed care/delegated. Will Milliman/MDHHS be specifically indicating what exactly is considered to be managed care/delegated administration? | 4/23/2021 | The SCA report documents functions that are considered managed care administration based on federal guidance and the MDHHS-PIHP and MDHHS-CMSHP contracts. Additionally, other administration (e.g., General Administration) will be allocated to both managed care administration and provider administration based on certain allocation methods outlined in the report that were determined to be appropriate by the SCA Workgroup. CMHSPs should also review their delegation agreement with their PIHP for additional details on what managed care activities they are responsible to provide. MDHHS and Milliman are available to provide guidance on managed care administration definition and allocation. |
| 41 | Managed Care Administration | For managed care/delegated admin, will Milliman be specifically listing what admin expenses are to be tracked under this? Or will Milliman be changing the direction for CMHSPs on this and allowing CMHSPs to allocate all admin as a provider of service? When will that decision be made? | 4/23/2021 | Please see the table in the Standard Cost Allocation Methodology Report mapping the non-encounterable cost centers to the administrative cost categories, particularly “Shared managed care administration – all other managed care administration” and “Shared managed care administration – healthcare quality improvement activities.” The functions in non-encounterable cost centers that map to these administrative cost categories are considered managed care/delegated admin. |
| 42 | Allocation Clarifications | On the EQI UNC tab, are we mandated to use a grant fund source in our EMR and track units of service? We currently track grant revenue and offset expense, but we do not track units of service. | 4/23/2021 | The grant fund source was included within the EQI template to allow for CMHSPs to capture units that are fully covered by grant funding. To the extent that a CMHSP does not provide any services fully covered by a grant fund source, then there would be no units reported under this source. Future COB reporting requirements will necessitate tracking grant funding offsets at the individual claim level. |
| 43 | Managed Care Administration | Under the cost center ‘Other Managed Care Administration’, what is meant by provider directory? How does that differ from Provider Network? | 4/23/2021 | Provider Directory is intended to represent the costs of compiling and presenting the details of your provider network in either electronic web-based or paper manual format for beneficiaries to find providers in your service area. We agree that this aligns with the activities under the Provider Network non-encounterable cost center and have moved it from “Other Managed Care” to “Provider Network.” |
| 44 | Assignment of Salaries and Wages | We have a Medical Director, would that position fall under General Administration or Clinical Supervisor? | 4/23/2021 | Medical Director costs fall under the Standard Expense Category “Salaries and Wages, Administration” which is next directly assigned to the non-encounterable cost centers. In general, Medical Director activities would fall under “General Administration.” However, depending on the activities of your Medicaid Director, some may be dedicated to one administrative function and all their salaries and wages will be directly assigned to the corresponding non-encounterable cost center. Other employees may support multiple administrative functions (or even have a mix of clinical and administrative responsibilities), which will require their salaries and wages to be assigned to the appropriate cost centers as a percentage of time spent performing the different activities. Activities that account for five percent or less of an employee’s total time are not required to be tracked or assigned to non-encounterable cost centers to focus efforts on splitting time associated with significant roles and responsibilities. |
| 45 | Non-Encounterable cost center clarifications / changes | In the 12/9/20 Standard Cost Allocation Methodology Draft document, under the non-encounterable cost center descriptions, there is an item called ‘Supervision’. The definition is between ‘Trainers Net Expense’ and ‘Medical Records’, however we didn’t see a cost center for this in the 200 series of numbers, would it be 218? | 4/23/2021 | Clinical supervision is cost center 301 |
| 46 | Service Cost Centers | Would a Program Director, a clinical position supervising 1st and 2nd line supervisors of direct run programs be assigned to the cost center ‘Supervision’? | 4/23/2021 | A Program Director, whose primary responsibility is overseeing program services, including overseeing the 1st and 2nd line supervisors of clinical services, should not be assigned to supervision, and instead should be assigned to the Standard Expense Category “Salaries and Wages, Administration” which would then be directly assigned to a non-encounterable cost center, likely General Administration. |
| 47 | Assignment of Salaries and Wages | If finance staff, such as a claims processing clerk, has a portion of their time allocated to 210/Managed Care Admin and to 204/Finance, would the CFO’s time be split between 204/Finance and 210/Managed Care based on the staff supervised? | 4/23/2021 | Leaders of administrative staff should allocate their time based on the activities they directly perform as individuals, not that of their staff. If a CFO spent 15% of their time reviewing/monitoring claims payment activities and 85% of their time on financial reporting and expense management, they would allocate their time to those non-encounterable cost centers as such, regardless of the percentage of their staff’s actual time allocation. |
| 48 | Non-Encounterable cost center clarifications / changes | For cost center 214/Quality, 208/IT and 210/Managed Care, where do you draw the line for quality data collection? When is it quality, vs IT or managed care? | 4/23/2021 | Activities that support ensuring 1) standards for staff, program and management performance exist; 2) compliance with them is assessed and 3) ongoing improvements are introduced, monitored, and assessed with respect to their outcomes should be assigned to the non-encounterable cost center "Other Healthcare Quality Improvement Activities" which is then assigned to the administrative cost category "Shared managed care administration - healthcare quality improvement activities." While a managed care administrative activity, it is necessary to separate out activities that improve health care quality for inclusion in the medical loss ratio. 45 CFR 158.150 provides additional clarification on what activities can be included in “214/Other Quality Improvement Activities.” Quality data collection will likely be allocated to 214 unless it is supporting one of the excluded activities in the statute, i.e. utilization management. |
| 49 | Non-Encounterable cost center clarifications / changes | Would a person that monitors Hab Supp Waivers, SED Waivers and Children’s waivers, assisting with recerts and etc. be considered to fall under 201 Access or 210 Managed Care? | 4/23/2021 | More information about the described individual's responsibilities may be necessary to determine their expense allocation. Activities assigned to the non-encounterable cost center "Access" should align to MDHHS' policy "Access Standards" as documented in the MDHHS-PIHP and MDHHS-CMHSP contracts. Clinical screening as part of determining coverage eligibility is a requirement of the Access policy and therefore those activities would be allocated to "Access." When not included in an encounter, monitoring waivers would be allocated to the non-encounterable cost center "Care Coordination." Both "Access" and "Care Coordination" are assigned to the administrative cost category "Shared managed care administration;" however, "Care Coordination" counts as activities that improve health care quality and can be included in the numerator of the medical loss ratio. |
| 50 | Assignment of Salaries and Wages | Would all of a medical assistant or nurse’s non-encounterable time be coded to 202 Care Coordination? Or would their time spent related to a psychiatric dr visit be coded to the 118 Psychiatric Services cost center? | 4/23/2021 | If the indirect, or non-billable time of a medical assistant or nurse is incurred to support the provision of a clinical service, it should be assigned to the clinical service or cost center being supported by the employee. If a medical assistant or nurse is supporting services that meet the definition for Psychiatric Services – Med Clinic, their time should be coded to that cost center whether or not their time results in a billable service. The direct and indirect time for these individuals is included within the independent rate model for this service and would be included in the Salaries and Wages - Clinical direct service staff expense category and included in the Med Clinic cost center. The non-encounterable cost centers should be used only when an employee’s time is not intended to be supporting the direct provision of a clinical service. Please refer to the definitions for the non-encounterable cost centers. |
| 51 | Non-Encounterable cost center clarifications / changes | It appears that cost center 208 IT is 100% allocated as general business operations expense, except for the portion attributed to encounter data, is that correct? Currently we allocate about 75% of the IT costs to direct run services based on IT staff time. | 4/23/2021 | The Methodology does separate encounters from general IT and includes encounters in the “other managed care administration” non-encounterable cost center which is mapped to the administrative cost category “Shared managed care administration – all other managed care administration.” Other IT activities in the non-encounterable cost center “IT” are mapped to the administrative cost category “Business operations” which is then further allocated to all cost centers based on the number of FTEs attributed to each cost center. |
| 52 | General | Is it expected that 100% of a CMHSP's expenses, that are also reported on the FSR, will also be in the Standard Cost Allocation Document? If not, what is excluded? |
4/23/2021 | There is an "Other" section in the FSR that may not be captured currently in the SCA methodology. Additional changes to the SCA model may be needed to capture these expenses. |
| 53 | Allocation Clarifications | For Montcalm Care Network employees, PTO earned in a year can equal between 10% and 16% of their annual hours paid of 2080, based upon years of service. Currently when PTO is paid it is charged to their "home" cost center, which is the cost center where the majority of their time worked is charged. At the end of the fiscal year the balance of unused leave is placed in a Leave Reserve fund, with increases or decreases from the previous years balances charged to the employees " home" cost center. These increases or decreases are accrued as wages, employment taxes to the home cost center. This is to assure funds are available should MCN go out of business to pay off employees for their earned PTO balance. What is Milliman's position on this? |
4/23/2021 | Without fully understanding the Montcalm Care Network PTO policy, the salaries and wages to be accounted for in the standard cost allocation should be the same as the salaries and wages expenses that have been accrued by the entity for the reporting period. In other words, if the increases or decreases to the Leave Reserve fund are accrued by the entity as wages in the reporting period, and the entity has determined that such accrual is consistent with GAAP, then those accrued wages should be included in the salaries and wages reported in the SCA worksheet. |
| 54 | Assignment of Salaries and Wages | Montcalm Care Network has 3 team leaders. The first is a Case Manager who spends 50% doing direct case management services, and 50% supervising several Peer Support Staff in the Peer Support Cost Center. The second is a Home Based Specialist who spends 20% supervising five Family Support Assistants who work in the Home Based Cost Center, and spends 80% doing direct home based services in the Home Based Cost Center ( all are billed for the same CPT code). The third works in the Access department where she supervises the front desk staff (Support Staff cost center) consumer registration ( Consumer Registration cost center) and coordinates the clinical staff who work in the Access Department (Access cost center). My question is how should these 3 staff be classified as far as which salaries and wages expense account to use? Should they split time between direct services and supervision or just choose one or the other? The third team leader is problematic because most of her "supervision" is of staff whose wages would be in the 05 salaries and wages expense and should the portion of her supervision time for the non-clinical go to 05 (do not provide direct services), portion of supervision time for clinical go to 02, and the balance of her time go to 01? Also is all Access staff time considered salaries and wages expense code 01? |
4/23/2021 | All salaries and wages for clinical employees, i.e., those that meet the definitions for Clinical Direct Service Staff or Clinical First- and Second-Line Supervision, should be classified as Expense Category 01 or 03, respectively. For clinical employees, time should be apportioned between 01 and 03 based on the time spent by employees. All salaries and wages for administrative employees, including Access, should be classified as Expense Category 06. For employees that have a mix of clinical and administrative responsibilities, it will be necessary to apportion their salaries and wages between clinical (01 and/or 03) and administrative (06). Apportionment should be based on time spent by these employees. For clinical staff, in addition to assigning salaries and wages to the appropriate Standard Expense Category (01 or 03), it is also critical to assign their wages and FTE statistics to the appropriate Standard Cost Center. Clinical staff wages (01) and FTE statistics should be assigned to Direct-run Clinical cost centers 101 - 139 (or to Excluded Services 401-403) based on the employee time spent. All first- or second-line supervision wages (03) and FTE statistics should be assigned to cost center 301, Clinical Supervision, (or to Excluded Services 401-403) based on the employee time spent. Administrative staff wages for employees who support multiple administrative functions should be assigned to non-encounterable cost centers 201-218 (or to Excluded Services 401-403) based on the employee time spent. For purposes of assigning wages and time, activities that account for five percent or less of an employee’s total time are not required to be tracked or assigned to non-encounterable cost centers to focus efforts on splitting time associated with significant roles and responsibilities. |
| 55 | Assignment of Salaries and Wages | Currently Montcalm Care Network allocates supervisors based upon the FTE's of the staff they supervise based upon the budget for the fiscal year. There are currently 12 such staff. Given MCN's 25% staff turnover and an average of vacant position per month, it would be very time consuming to update supervised actual staff FTE's every month before allocation each supervisor. Each supervisor has their own cost center where their costs are accumulated before allocation each month. Each supervisor has their own allocation expense account that posts their allocation amounts to the cost centers where their staff charge their salaries and wages. At that point you cannot tell the breakout of the supervisor's allocation by the proposed 19 proposed SCA expense accounts. I am not going to post these allocations by the up to 19 proposed SCA expense accounts. This means that the 02 expense account will for the most part only appear in these individual supervisor's cost centers and not in the cost centers where direct services are provided. Which of the 19 expense accounts would these allocations of first and second line supervisors be included? |
4/23/2021 | See response to above question. |
| 56 | Service Cost Centers | Service codes 96130 & 96131 are cross walked to cost center 113 on Appendix 2. How should service codes 96130 & 96131 be coded to Autism, which is cost center 102? | 4/23/2021 | These services are not specific to Autism and therefore are not being included in the Autism cost center. |
| 57 | Service Cost Centers | Service code H0032 is cross walked to cost center 105, case management. If T1016 & T1017 are inclusive of treatment planning (H0032), why is H0032 only listed under cost center 105 case management? | 4/23/2021 | The SCA Workgroup has updated the cost centers for this and other services. |
| 58 | Service Cost Centers | Why doesn’t cost center 109, Crisis/Mobile Crisis, include service codes H2011 & T1023? | 4/23/2021 | We have discussed this issue with MDHHS and will be utilizing H2011 HT to identify Mobile Crisis services for children and adults. All other crisis services will be included in the Crisis cost center, which is separate from Mobile Crisis. |
| 59 | Allocation Clarifications | Will the new education modifiers be required for FY22? How will these education modifiers be used for reporting and cost allocation? | 4/23/2021 | The provider group modifiers will be required for all non-team based services beginning in SFY 2022. These provider groups, however, are not required to be tracked in the CMHSP general ledger. Service costs are accumulated in the clinical cost centers and the model creates establishes a composite cost per minute for each cost center. The weighted average cost per minute method (which is described in the SCA Methodology report in detail) utilizes the provider group modifiers and standard weighting to allocate costs to each procedure code/provider group modifier combination. |
| 60 | Allocation Clarifications | Do CMHSPs only do direct-run services for third parties? Need to think about administration allocated to third-party expenditures. What happens to the administrative costs for the GF or Third Party claims? The CMH manages the provider network for all benefits regardless of payer. i. There will be administrative costs for GF ii. Effectively, the admin will never be allocated to third-party payers and will fall on GF or Medicaid. Is this allowable? Can you say more about the 3rd party payor comment you made please. Will need to talk through as a work group and whether acting as an entity subcontracting to other providers or only serving third party payer as a provider to further refine the methodology. |
4/23/2021 | Managed care administration will be allocated to all payers; it was noted that this will be minimal for non-Medicaid payers during SCA Workgroup discussion on 2/12. Further discussion needed for Commercial/Medicaid payers. |
| 61 | Non-Encounterable cost center clarifications / changes | What about insurance buyout payments (healthcare opt out)? Is this considered compensation? | 5/26/2021 | If CMH is accounting for this as an insurance expense (by GAAP), the way it is classified, is how to include the expense in the SCA model. |
| 62 | Non-Encounterable cost center clarifications / changes | What about employer contributions to Health Savings Accounts? Should this be treated the same as healthcare expense? | 5/26/2021 | Employer contributions to HSAs are treated like insurance. |
| 63 | Non-Encounterable cost center clarifications / changes | How about employee EAP and wellness program expenses? | 5/26/2021 | EAP is considered an HR function, which is allocated by FTE. |
| 64 | Non-Encounterable cost center clarifications / changes | How PTO is handled when it is deferred? | 5/26/2021 | Federal guidance 200.431 section B includes leave, including PTO, as allowable if all criteria met, and costs equitably allocated. |
| 65 | Service Cost Centers | Is 108 just for Youth Mobile Crisis and 106 for both State Certified Intensive crisis and other crisis? Is the intent to keep Youth crisis separate from other crisis or to keep a State Certified Intensive Crisis program (that can serve both youth and adult) as a cost center? | 5/26/2021 | Cost center 108 is for mobile crisis only, while all other forms of crisis should fall under cost center 106. Based on the new SFY 2022 code sets, any crisis codes with an HT modifier will fall under 108 Mobile Crisis, while all non-HT crisis codes will fall under 106 Crisis. The following are notes from the 5/26/2021 bi-weekly meeting: Feedback was provided that State Certified Intensive Crisis program (which was described as mobile crisis for adults) includes MD time, which is billed under S9484. S9484 code is in 106, but should be within 108 along with mobile crisis. MD is called in as needed and is also paid for on-call even if they do not provide services. Other qualifying providers use the S9484 code as well, e.g. social workers, and this is also corresponding to mobile crisis. Youth mobile crisis (24/7) will also use HT, but an MD is not required on call for this team. CMHSP also has a crisis team separate from mobile crisis (Emergency Crisis Response Team). This team does things such as a preadmission screening, but does not follow-up after the initial contact like the mobile crisis teams are required to do. There will be follow-up discussions with MDHHS and the SCA Workgroup confirming the proposed change to include S9484 in the mobile crisis cost center. |
| 66 | General | Is it expected that the SCA will show an allocation of expenses by funding source, or is that not determined until the information is entered into the EQI? The current cost allocation plan I use takes costs from the GL by cost center after various allocations have been made in the GL ( fringe benefits, vehicles, IT, space, fringe benefits, IT, supervision). Then I run a service activity log data report for the period which breaks out services by cost center by funding source. From this report I calculate funding source percentages by cost center and apply them to the accumulated costs in the cost center. From this I determine the overall cumulative funding source revenue earned (Medicaid, HSW, SEDW, Healthy Michigan and General Funds). I do not do this by individual HCPCS code. The resulting revenue breakdown is then booked to the General Ledger for the period. As a result, I can run revenue and expenditure reports from the General Ledger for each cost center. I would plan on continuing to do this starting 10/1/21. I would still use the cost allocation plan I currently use. I would be internalizing as many of the SCA allocations in my General Ledger, just entering the resulting allocations by cost center for each in the SCA. Those costs that are allocated only in the SCA would then be booked to the General Ledger. At this point the costs in each would be distributed the same. I would then run the same service activity log reports that I have used before to determine the break down by funding source. |
5/26/2021 | The SCA Workgroup discussed that many CMHSPs are internalizing the standard allocation methodologies. To accommodate this, the SCA model allows CMHSPs to directly allocate all expense categories if allocation methods are internalized. It is unclear whether the methodology you have implemented using the service activity logs follows to weighted average cost per minute method. If it does not, then your internal expenditure reporting would not be consistent with the results of the SCA model. The following are notes from the 5/26/2021 bi-weekly meeting: CMHSPs should track both the direct and indirect time attributable to the service and assign the service related time to the appropriate cost center. Indirect time not attributable to services should be allocated based on the sum of direct and indirect service related time. There was clarification that direct minutes were utilized from the encounters on the Service UNC tab in the SCA methodology. Services that do not include enough time to result in an encounter would not be included in the Service UNC tab, but should be included in the cost center. |
| 67 | Service Cost Centers | On the updated Appendix 2, we’re not seeing the following: T1016, and hospital codes such as 0100,0124, 0912, 0913. What cost center would these fall under? | 5/26/2021 | T1017 is the only service code used for case management and supports coordination beginning in SFY 2022. An update to Appendix 2 will list out all services that are understood to be always contracted out to network providers and thus not necessary for the direct-run cost allocation. Appendix 2 updates will include services assumed to be contracted only. |
| 68 | Non-Encounterable cost center clarifications / changes | Should we split out prevention and advocacy from other mental health code functions? | 5/26/2021 | Prevention and advocacy will be included as separate lines in future EQI reporting for the Mental Health Code expenditures that are captured within the Mental Health Code/CMHSP Only Activities non-encounterable cost center. |
| 69 | General | Is the costing process expected to update the EQI only on the annual report or each time the EQI report is submitted during the fiscal year? | 5/26/2021 | It would be updated each time the EQI report is submitted, every four months. It is anticipated that inputting the trial balance should not be a significant time commitment. |
| 70 | Assignment of Salaries and Wages | What do you use for Team Leader wage expense account? 1 or 3? | 5/26/2021 | Reference Slide 24 from the April 2021 training. Team leads might have overlap in these expense categories used. For example, a home based worker leading peer support (different cost center); part of their time in expense category 01 attributable to home-based services and of their time in expense category 03 attributable to supervision of peer support. |
| 71 | Managed Care Administration | I'm still trying to make sure we handle Managed care admin correctly, we are a CMH that direct runs over 90% of our services- not all our Admin should be Managed care admin - right ? For example, how much of total Accounting Admin cost is attributed to service provision and how much is managed care admin ? | 5/26/2021 | That is correct, not all admin should be managed care. Certain non-encounterable cost centers (e.g., Finance) will be allocated to both managed care admin and provider admin. Slide 16 (April training) and SCA methodology report provides more information on allocation methods. CMHSPs with mostly direct-run services will have more of their business operations attributable to provider administration than a CMHSP who contracts out most of their services. |
| 72 | Service Cost Centers | Would it be possible to have a complete list of cost centers with definitions, the standard expense categories and their definitions and the HCPC/CPT code crosswalk to the cost centers all in one document? We are having difficulty switching from document to document as we work through this new methodology. Thank you! | 5/26/2021 | Thank you for the suggestion. The next version of the report will include an Appendix with all of the cost centers and definitions in Appendix 2. |
| 73 | Service Cost Centers | An issue we stumbled on as we work through the new methodology and are having difficulty solving is for the service codes that can be coded to two different cost centers such as 112/117. To be able to select the cost center based on the new education level modifier in our EHR, the modifier will need to be added on the backside at an earlier stage in the process. Currently backside added modifiers are added at the time a service becomes and is reported as encounter. To use this modifier in a GL mapping in a PCE system, the assignment will need to occur before the adjudication of claims. We don’t know if this is possible, but wanted you to consider this issue to see if there are any other solutions you may be able to come up with. | 5/26/2021 | We would request at least one CMHSP work with their EHR vendor regarding this issue and share the resulting solution or further defined issue. MDHHS would be happy to facilitate a meeting to reach a solution on this topic if discussions between CMHSPs and EHR vendors cannot create a solution that can be shared with all CMHSPs. |
| 74 | General | Has Milliman/MDHHS been working with the various CMHSP/PIHP software vendors such as PCE to see how they can assist with implementing this new methodology? | 5/26/2021 | SCA workgroup members made best effort to consider system changes needs in the design of the SCA methodology; however, EHR vendors have not been involved in the discussions to date. Please also see the response to the question above. |
| 75 | Service Cost Centers | We are beginning the process of aligning our EHR to the proposed standard cost allocation cost centers. I found some issues with the current version of appendix 2. • Autism – Should include H0031U5 • Supports Coordination (T1016) is not listed in any of the cost centers • 90792 is not listed in the Psychiatric Services – Med Clinic & Outpatient for MH (it is included in SUD) • H0031 is only listed in SIS Assessment with WY modifier. This code is used for services other than the SIS Assessment Please let us know if these changes will be implemented. |
5/26/2021 | There are several updates related to the identified codes. 1. Appendix 2 released in April 2021 included 90792 for both mental health and SUD cost centers. 2. H0031 will have a redefinition of qualified providers. The WY modifier is appended to H0031 to indicate SIS, but nonprofessional assessment for the reduced list of qualified providers is still included. Crosswalk has been developed. Provider qualifications will need updated. Noted that ADOS will use 96112/113. 3. U5 modifier has been removed from the SFY 2022 code sets 4. T1016 has been removed from the SFY 2022 code sets. All case management will be coded under T1017. |
| 76 | Service Cost Centers | Discussion of consolidation of SUD and Non SUD Cost centers. Proposal is to remove SUD-specific cost centers and to blend them with MH cost centers. |
5/26/2021 | CMHSPs can have more detail than the SCA cost centers if they choose, but discussion was that we don’t want to require the additional detail in the SCA framework. There was a question about whether encounters would be impacted. SCA Workgroup did not believe encounter reporting would be impacted by this change. SCA Workgroup to work with select CMHSPs who suggested the change to determine what cost centers should be utilized/retained for SUD service codes that do not have a corresponding MH service code (e.g., H0015, H0019) Please let the SCA workgroup know if you are aware of any reporting requirements that may not mesh well with this change |
| 77 | General | Discussed use of H2015 by peers who are not yet certified. | 5/26/2021 | The state will be reviewing what is included in the reporting and costing considerations and determine if peers should continue use of H2015 before certification. |
| 78 | General | Any idea when the "Draft" will be considered final? We want to begin cross walking our current account strings but there are over 15,000 of them so we don't want to have to do it several different times. |
5/26/2021 | There should not be significant changes from the version shared at the April training. The goal is for no more major changes to the expense categories and cost centers, except for the consolidation of SUD cost centers. CMHs should be able to start without too much burden coming later from other changes. It is expected that there will be ongoing changes as needed, e.g. when codes are updated. |
| 79 | Allocation Clarifications | Currently each manager has their own cost center. Their wages and benefits, allocation of IT, space and other directly charged costs related to them are accumulated in their personal cost center. At the end of the month the costs in their cost center are allocated to other cost centers based upon the budgeted FTE's of the staff they supervise. The SCA is now requiring that they be allocated based upon where they actually spend their time by cost center. For allocated Health insurance the SCA requires that this be based upon the FTE's of all staff eligible and participating in the insurance plan. This can be determined at the beginning of the year and applied throughout the full year. I have absolutely no basis to allocate mangers time by activity for various cost centers, other than the FTE's of the staff they supervise. Using the Case Management cost center as an example. As the FY 2021 begins, if managers are now charging their time to various cost centers every day, there will be three managers using the 03 Standard expense category code charging to case management. Each of these also supervise staff in other cost centers. I can no longer keep track of each individual manager. |
6/10/2021 | The SCA methodology does represent a different approach than the method described in this question. The SCA workgroup has established a method that assumes it is reasonable for CMHSPs to assign direct service staff wages to Standard Direct-Run Clinical Cost Centers based on the types of services they provide, and to assign administrative staff salaries to Standard Non-encounterable Cost Centers based on the nature of the administrative functions they provide. Facility-related costs should be allocated based on the square footage use of space for each standard cost center. Other directly charged costs should also be assigned to standard cost centers based on their purpose. If managers meet the definition of first or second line clinical supervision, their salaries and wages should be accumulated and assigned to the single Clinical Supervision cost center (301), where they are further allocated to clinical cost centers based on the relative salaries and wages of clinical staff. If managers fulfill an administrative function (i.e., they do not meet the supervision definition, nor do they provide billable clinical services), their salaries should be allocated to one of the standard Non-encounterable cost centers. The employer portion of employee health and other insurance-related expenses, pension expenses, and other fringe benefits should be allocated to all cost centers based on allocated employee salaries and wages. Payroll taxes and fees should be directly assigned to each cost center based on the assigned employees (i.e., payroll taxes and fees should follow the employee). |
| 80 | Assignment of Salaries and Wages | Do you expect each of the 6 expense categories for wages to remain specifically identifiable throughout the allocation process? First example. First and second line supervisors. Supervisor A costs are accumulated in a separate cost center for Supervisor A. Supervisor A wages are charged to expense 03. On a monthly basis, all of the costs are accumulated related to Supervisor A in the Supervisor A cost center, including fringes (expense accounts 07, 08 and 09), space (expense code 17) and other such as IT (expense account 20). On a monthly basis all of the costs in the cost center for Supervisor A are allocated to the staff that are supervised. Supervisor A supervises Case Managers who split their effort between case management services in costs center 104 (Case Management) and family training in cost center 113 (Outpatient). For example, this might be 90% to 104 and 10% to 113. Currently when this allocation is booked to the General Ledger, there is an expense account entitled allocation of Supervisor A. The entry to book this zeroes out the amount in the Supervisor A cost center and shows amounts in cost center 104 and 113 for one amount allocated to each of the cost centers. All of the distinctions of expense accounts disappear and are consolidated in the allocation of Supervisor A expense account. If we continue to follow this process in the SCA it will not reflect any 03 expenses. The same would be the case for all of the administration costs in the 200 cost center series. If all of the expense accounts must keep their detailed expense code this will be a big problem. It will be nearly impossible to put the genie back in the bottle, that is translate back to the General ledger what was done in the SCA. |
6/10/2021 | The expense categories are not specifically identifiable throughout the allocation process, but they are identifiable within the summarized trial balance. Expense category 03 is for staff supervisors and 05 is for contractual staff as supervisors. Both get allocated solely to cost center 301 regardless of the cost center included within the trial balance. Cost center 301 is then allocated proportionately across all clinical cost centers. There is not a need to track individual clinical cost centers that supervisors are supervising, but that can be done in the CMHSP general ledger if the CMHSP opts to do so. |
| 81 | Service Cost Centers | From the current list of cost centers, I fail to find what cost center(s) to use for Contracted Clinical Services. The cost centers listed with matching HCPCS codes in Appendix 2 are identified in the Draft Standard Cost Allocation Model as of 5-11-21 in the CMHSP Cost Center Group column as " Direct-Run Clinical". Would these be reported under 211 Provider Network? The only place I see a "Contracted" designation is on the Service UNC tab in the Draft Standard Cost Allocation Model received 5-11-21 in column O "Standard Cost Center". But all of those so designated in Column O only pull costs from other worksheet tabs in the model to Column X "CMHSP Direct-Run Expenditures". The column where I would expect to see contracted expenses, which would be column Y "Network Provider Expenditures", has no formula and is blank. I believe "Direct-Run Clinical" costs need to kept separate from "Contracted" due to separate types of allocations. |
6/10/2021 | The SCA methodology is primarily intended to allocate costs incurred by CMHSPs to either direct run clinical services or to administrative functions. Contracted network provider services do not have any cost center requirements, but can utilize the existing cost centers if a CMHSP opts to do so. The contracted network provider service costs and units should be directly assigned based on the service codes actually billed for and paid by the CMHSP. Amounts paid by CMHSPs to contractors that provide administrative services should be directly assigned to the appropriate non-encounterable cost center. The Service UNC tab and recent SFY 2022 code set documents have included a SCA Cost Center column. In some cases, this is listed as "Contracted". This indicates that the SCA Workgroup does not believe this service is ever delivered directly by CMHSP staff and therefore is not included in one of the standard cost centers. |
| 82 | Service Cost Centers | For contracted clinical encounterable services, what cost centers should be used? Are you planning to add additional numbers that correspond with the 101-138 that contracted services will be coded to or can we make up our own, maybe the 600 series? The 4/26/21, page 6, SCA Methodology – April Training says that under std exp cat 10, it does list cost centers 101-139 – does that mean we can use those even though other documents say direct-run only? | 6/10/2021 | See above response. |
| 83 | General | Will CCBHC be added into the model? | 6/10/2021 | SCA Workgroup is working with MDHHS to review and understand the CCBHC reimbursement methodology and reporting requirements as they intersect and relate to the SCA methodology. MDHHS is currently working with CMS on the reporting requirements and further discussion will be shared in the future. CCBHC services are a subset of CMH services, so no additional cost centers or expense categories should be necessary. Other reporting needs are being considered. Changes to the SCA structure/cost centers are not anticipated. |
| 84 | Non-Encounterable cost center clarifications / changes | Clarify IT allocation | 6/10/2021 | IT costs follow the non-encounterable cost centers allocation process. Staff allocated to 208 are then allocated to business operations and spread to all other cost centers based on FTE count. This allocates hardware, software, and technical support services across all employees with the assumption that every employee has some level of technical infrastructure support. Timesheets or other time mechanism is critical to assigning time to the appropriate cost centers. |
| 85 | Expense category strategy | Can you define what you include in first and second tier supervision again? | 6/10/2021 | Some organizations create two tiers of supervision. Whether organizations have one or two tiers of supervision, the assumption is that it is generally a 1:10 ratio (except for EBPs). Some may have 8 first line supervisory with 2 second-line supervisors (i.e., this is not a program director). This language was intended to provide flexibility in the staffing model that some CMHSPs were known to have. |
| 86 | Non-Encounterable cost center clarifications / changes | What cost center should consumer registration go in? Access or Customer service? What cost center would reimbursement/billing staff go in? They deal with direct run services as well contracted services. Where would recipient rights go now that Milliman knows it is not all Mental Health Code/CMHSP Only Activities Unique non-encounterable CMHSP only activities (e.g., MHC) that are assignable to Medicaid, Healthy Michigan and GF? What cost center would the executive director go in? |
6/10/2021 | Please refer to the MDHHS Access Policy and MDHHS-PIHP contract and review the consumer registration activities to determine if they are "Access" or "Customer Service" or "General Administration." Reimbursement/billing staff would be assigned to "Finance" which requires further allocation to all other cost centers as a percentage of the total expenses directly assigned or allocated to each cost center. This presumes the greater the size of the functional area, the greater the consumption of financial services. Recipient rights and other mental health code/CMHSP only activities that are not captured by a service code should be allocated to this cost center. These expenditures will be allocated to Medicaid, Healthy Michigan, and/or General Fund based on total allocated expenses. Executive Director would be assigned to "General Administration" which requires further allocation to all other cost centers as a percentage of the total expenses directly assigned or allocated to each cost center. |
| 87 | Service Cost Centers | In the SCA Q&A 20210527.xlsx file on line Row 73, it says: “CMHSPs should track both the direct and indirect time attributable to the service and assign the service related time to the appropriate cost center. Indirect time not attributable to services should be allocated based on the sum of direct and indirect service related time.” Does this mean it should be tracked in payroll? Or through Service Activity logs? There was clarification that direct minutes were utilized from the encounters on the Service UNC tab in the SCA methodology. Services that do not include enough time to result in an encounter would not be included.” Is this second statement the clarification? | 6/10/2021 | How to track direct and indirect time will be a CMHSP decision based on a number of different factors. The SCA Workgroup requests that any CMHSP needing training and/or technical assistance reach out to SCA.Feedback@Milliman.com. Once there is an understanding of the number of CMHSPs requesting assistance, a plan will be put together to provide that assistance. We've clarified a sentence in row 73: Services that do not include enough time to result in an encounter would not be included in the Service UNC tab, but should be included in the cost center. |
| 88 | Allocation Clarifications | Am I understanding that health insurance would be allocated based on wages where higher paid staff would be charged with a higher percent of the health insurance cost? | 6/10/2021 | Higher paid staff are paid with higher percent of costs, but the goal is consistency. We will evaluate after one year, and this may change in the future. While a higher portion of insurance costs are covered by higher paid staff, the same percentage should be applied to all salaries and wages. Individual costs are higher, but the percentage should be the same. |
| 89 | Allocation Clarifications | Am I understanding correctly that health insurance would be allocated to wages of staff who do not receive health insurance because it based on wages and not based on wages of staff actually receiving health insurance benefits, for example relief staff, temporary staff or staff that do not qualify for insurance benefits? | 6/10/2021 | Yes. There has been some discussion with the SCA workgroup. Originally we looked at basing the allocation on qualifying FTE to attribute expenses to those employees eligible to receive the benefits. After audit concerns were raised with the qualifying FTE approach, the SCA workgroup determined that attributing based on all employee salaries and wages was the most viable option for consistency, understanding that not all will take insurance. |
| 90 | General | At what frequency would the percent of wages be able to be calculated? | 6/10/2021 | Some CMHs may recalculate monthly to match grant monthly cycles. Some CMHs may recalculate every 4 months with EQI cycle. One suggestion is to consider doing monthly. |
| 91 | Expense category strategy | How to input if we currently directly assign benefits? | 6/10/2021 | The SCA methodology was revised to allocate insurance benefits based on all employee salary and wages. CMHSPs may have to make changes to comply with the SCA methodology. Each CMH will need to evaluate what they need operationally. Some CMHs may want to directly assign benefits into the cost center, e.g. due to Board reporting, but for purposes of Medicaid reporting they will have to comply with the SCA allocation methodology. This is an area of CMH choice based on other reporting requirements. Expenses can be input in the standard summarized trial balance in the SCA model as direct assigned to cost centers or without allocation to cost centers. If the assignment to cost centers used in the CMHSPs General Ledger for this expense category is not consistent with the SCA methodology, these expenses will need to be allocated within the SCA model (i.e. by changing the input in E11 on the Expense Category Summary tab). If the assignment in the CMHSP General Ledger is consistent with the SCA Methodology, they can "directly assign" the expense category (this option is only applicable for 08 Insurance, 09 Retirement, and 17 Facilities). The CMH should make sure the allocation used in the model aligns with the SCA methodology and flows through to unit costs, which will then be used for EQI reporting. |
| 92 | General | I understand this for the costing allocation, but to see the true costs of a cost center from a business perspective, this will skew our financials when reporting to our boards, and programs. Is the expectation to have this occur for our financials and change our methodology for reporting? | 6/10/2021 | This question has been discussed in the SCA workgroup. A few CMHs already do direct assignment that follow individual person. The CMH has flexibility to report to Board and/or grantor agencies, so the CMH has the ability to do direct assignment (follow individual for the reporting with no expectation that Board reporting changes). Each CMH will make decisions on what their Board looks at for financial information. It was noted that there is value in having the board look at financials in the same was that the state looks at financials and will ask questions, but not a requirement. |
| 93 | General | During the last call, the removal of T1016 was discussed due to the similarities with Targeted Case Management (T1017). We have several Supports Coordinator Assistants that currently utilize the T1016 code—Per the provider qualifications document, they only require a high school diploma and one year of experience with proper supervision. Conversely, the T1017 code currently requires a QMHP, QIDP, CMHP, etc. If T1016 is eliminated, will provider/staff qualifications be broadened to allow usage of T1017 by Supports Coordinator Assistants that do not meet the QMHP/QIDP/CMHP threshold? | 6/10/2021 | T1017 has been updated to include the supports coordinator assistant, the broker, supports coordinator, and independent facilitator as qualified providers. |
| 94 | General | Will you please provide the rationale for H0032 being excluded from the Psychiatric Services – Med Clinic cost center? |
6/10/2021 | Milliman verified that H0032 has been updated to include both the Psychiatric Services - Med Clinic and Outpatient cost centers, depending on the provider qualifications. |
| 95 | Allocation Clarifications | We are working through the application of SCA in a Day Program environment, where we have Supported Employment (H2023), CLS (H2015) and Skill Building (H2014) services being provided. These services are being provided by the same direct care staff, in the same environment. Would it be possible for us to include all of these codes in a single cost center? There are some significant concerns with our team about the ability of direct care staff to accurately allocate this time between the various codes being provided, especially where they are frequently moving between the services based on the various consumers being served simultaneously. | 6/10/2021 | The SCA Workgroup discussed that CLS and Skill Building are performed by similar staff and have similar amounts of indirect time; Therefore, we have consolidated the two cost centers into a single cost center. It is our understanding that supported employment is not necessarily performed by similar staff as CLS and Skill Building, and it also does not have similar indirect time. MDHHS is working through providing additional clarity regarding Supported Employment services that will be added to the code sets in SFY 2023. |
| 96 | General | Should the FSR be implemented into EQI? | 6/10/2021 | There are no current plans to integrate the EQI and FSR. This can be discussed after talking to the SCA workgroup and MDHHS. Results revenue and expenses from the EQI are included within the FSR, but the FSR is broader in scope. |
| 97 | Allocation Clarifications | Question about SIS Assessors. We are a PIHP. We hire all the SIS assessors for our region and allocate the full cost back to the four CMHSPs in our region who reimburse us in full for the costs. Do we report the full cost of the SIS Assessors or do we report our net cost after CMHSP reimbursement of $-0-? | 7/7/2021 | This would be a contracted network provider service from a CMHSP perspective and would have offsetting revenue and expenses from a PIHP perspective. |
| 98 | Service Cost Centers | Why is H0045, respite per diem, split out to a separate cost center of 120? Why wouldn’t it be included in cost center #119? | 7/7/2021 | H0045 is a Respite per diem code and also a team-based service. The SCA Workgroup has separated team-based services from other services in many cases. |
| 99 | Grants | 1. Our CMH has various grants. Most of the services provided under these are not reported as encounters. The new grant cost center is 206, which is non-encounterable. That makes sense, however the EQI UNC tab does have lines to report grant. a. Three questions: a) are we to report grants where services are not included as encounters in the cost center 206? B) and then grants where we may have a few encounters would be reported under the program cost center that they fall under and units identified on the grant rows for the service codes? c) using this method our cost center 206 would not reconcile in total with the FSR grant sections, would this this be a reconciling item listed on the EQI ‘Financial Reconciliation*CMH’ tab? |
7/7/2021 | Grant expenses that are not fully covering a service identified with a corresponding encounter service should be captured in cost center 206. Expenses attributable to grants within a program cost center should be allocated to the corresponding service cost center. Encounter units fully covered by grants should be captured in the applicable grant rows of the Service UNC tab of the EQI. Total grant expenses would equal the sum of expenditures attributable to grant service units on the Service UNC tab plus the total non-encounterable grant cost center. Please also see prior related question. |
| 100 | Expense category strategy | Expense category for Worker’s compensation insurance and Unemployment expense | 7/7/2021 | Worker’s compensation insurance and Unemployment expense would fall under expense category 07, employee insurance costs. It is not necessary to allocate 07 Employee Insurance Costs in your internal accounting records. This allocation can be done automatically by the SCA model. To the extent that you would like to allocate Employee Insurance Costs in your internal accounting records instead of using the model, we would expect that you use the prescribed allocation methodology. There may be some expenses deemed to be immaterial within the expense category that would not be required to have a consistent allocation methodology (e.g., workers compensation). |
| 101 | Expense category strategy | Expense Category 10 – Network Provider Services, Clinical; is this for services provided by external providers and normally paid fee for service based on submitted claims? | 7/7/2021 | Yes. The SCA methodology is primarily intended to allocate costs incurred by CMHSPs to either direct run clinical services or to administrative functions. Contracted network provider services do not have any cost center requirements, but can utilize the existing cost centers if a CMHSP opts to do so. The contracted network provider service costs and units should be directly assigned based on the service codes actually billed for and paid by the CMHSP. Appendix 2 provides a complete list of the direct-run clinical cost centers and the corresponding CPT codes that should be used to map expenditures to each cost center. EXAMPLES: Purchased provider services (billable patient encounter, e.g. CPT/HCPCS code) from another CMH; purchased provider services (billable patient encounter, e.g. CPT/HCPCS code) from a community behavioral health provider. |
| 102 | Expense category strategy | Expense Category 11, Contracted Services, Administrative; Could this be a contract with another CMH for Access Center Services, or Customer Service functions? | 7/7/2021 | Yes. This category is for administrative amounts paid to outside entities (including individuals not employed by the CMHSP) for administrative services. This includes administrative services delegated to CMHSPs by the PIHPs, as well as business operations contracts. EXAMPLES: Information systems consulting services, Legal, management contracts, and overnight phone operating services. |
| 103 | Expense category strategy | Expense Category 12 - Contracted Services, Other; Would this be like Legal & Consulting? Auditing? | 7/7/2021 | If Legal and auditing are contracted services, they are reported under Expense Category 11, Contracted Services, Administrative. If this work is completed by CMHSP staff, it is reported in the Salaries and Wages, Administrative category. Consulting is also reported in the Expense Category 11. This category is for expenses paid to outside entities for administrative type services. Expense Category 12 – Contracted Services, Other is for services not included in either contracted clinical or contracted administrative services. Appendix 1 provides more detail. |
| 104 | Expense category strategy | Expense Category 16 – Clinical Program and Support Expenses; Would this be program supplies? Office supplies? | 7/7/2021 | Program specific supplies can be included in this category. General office supplies are captured in Expense Category 19, Other Expenses. Category 16 includes expenses incurred related to client related activity expenses. EXAMPLES: Non-billable medical supplies, and client and staff recognition supplies. |
| 105 | Allocation Clarifications | When entering data on the Standard Summarized TB, I noticed that the wages I entered for cost center 104 and cost center 204 caused column Q to show "S&W" while the wages I entered for cost center 301 showed "0". | 7/7/2021 | An issue was identified in the SCA Model based on this feedback. A revised version of the SCA Model will be provided later today with the issue corrected. |
| 106 | Allocation Clarifications | We have about a dozen different supervisors that I do not want to allocation them on this mass basis. I believe I heard previously that we could manually enter each one separately and not use the "mass" allocation based upon all cost centers. How would this be accomplished? | 7/7/2021 | Supervisory expenses are pooled in cost center 301 and allocated proportional to all clinical cost centers based on total directly assigned and allocated expenses. Supervisory expenses can not be done manually through the SCA model by design to eliminate variation in supervisory expenses across the state. |
| 107 | Allocation Clarifications | How do allocated Administration costs get to clinical contracted services on the SCA when there is no cost center for clinical contracted services? From what I can see, if I enter 100% of all of the admin cost center costs, but some portion needs to go to contracts, the allocations are based upon direct-run and other admin cost centers. If any of the administrative costs centers are related to contracts, either fully or partially, i.e., Finance, General Administration, Provider Network, Utilization Management, etc, from what I can see, there is no place in the SCA to allocate these costs away unless I use cost center 403, which is not defined for this purpose. | 7/7/2021 | PIHPs may only include in incurred claims the amount that the CMHSP or PIHP actually pays the provider/supplier for providing Medicaid covered services. Managed care rules defining MLR standards at 42 CFR 438.8 state that incurred claims must include the direct claims paid to providers and must exclude expenses for administrative services. Given these standards, the SCA methodology does not directly allocate administrative expenses onto clinical contracted network provider services. The SCA Workgroup has proposed to MDHHS a list of functions that could be retained as centralized provider administrative expenses by the CMHSP and included in contracted network provider incurred claims costs, including: • Centralized/Uniform Training (example: CMH maintains a training department and training curriculum specifically designed and maintained to meet the unique needs of the providers/staff, both inside the CMH and external providers, working in that community) • Electronic Health Record/Clinical Records system/Support staff (example: provider does not have internal system and therefore accesses/uses the CMH system including CMH tech support staff) • Space Costs (example: CMH encourages colocation for convenience of consumers and covers actual cost instead of requiring provider lease and increased service rate) • Fleet Costs (example: CMH purchases and maintains fleet but allows providers to utilize the fleet to both ensure appropriate maintenance/safety of vehicles and reduce cost at the provider) If MDHHS agrees with these business to business expenses, additional guidance will be provided regarding how to account for these expenses and how to report impacted encounters. |
| 108 | Allocation Clarifications | Our reimbursement staff deal with direct-run services and contracted services. Since you have defined what is the make up of each of the 200 series cost centers, we would have to split between direct-run and clinical contracted services. Finance pays clinical contracted services, but with no alternative to allocate to clinical contracted services, where does the amount related to this function go? | 7/7/2021 | The SCA methodology by design does not allow for administrative services to be allocated onto clinical contracted network provider services. Administrative expenses are pooled in the non-encounterable cost centers and allocated between direct-run provider administration and managed care administration. |
| 109 | Allocation Clarifications | Does the Trial Balance Validation summarize everything that has been entered on the Standard Summarized TB? Since there is no place to allocate clinical contracted services in the SCA you cannot enter these costs in the SCA? Thus, we cannot download our entire Trial Balance? | 7/7/2021 | The intent is to download all expenses on the Standard Summarized TB tab. The Trial Balance Validation intent is to summarize all of these expenses and to highlight (in red) if any expenses are assigned to cost centers that are not in line with expectations of the model. |
| 110 | Non-Encounterable cost center clarifications / changes | According to the PHIP and CMHSP Standard Cost Allocation Methodology, dated 4/23/21, page 16 there is a cost center listed for property., but I do not see that listed on Appendix 2 revised as of 6-11-21. Has that been eliminated? | 7/7/2021 | The property cost center has been removed. Property costs would be put under 403-Other. |
| 111 | Service Cost Centers | Is a contracted psychiatrist a part of direct-run services? | 7/7/2021 | Please refer to the definitions in the SCA methodology report regarding when contracted staff can be considered CMHSP "employees". If a contracted staff person, such as a psychiatrist, falls under the definition of employee as outlined in the SCA report, that person can be included as direct-run staff. |
| 112 | Service Cost Centers | Would it be possible to get one document, that includes tabs for all of the SCA pieces, such as cost centers cross walked to the service codes and another column that includes the cost center description. Also would it be possible to include a tab for the Standard Expense Categories and their descriptions? Maybe these tabs could be inserted in an updated SCA tool/worksheet so that we can easily access them? And add any other tabs with information that would be helpful? | 7/7/2021 | Appendix 1 provides the standard expense category definitions and examples and Appendix 2 provides the standard cost center examples. We will incorporate them into the next version of the SCA workbook. |
| 113 | Allocation Clarifications | Several questions/examples raised on the question of allocating administrative costs to contracted providers. General administration costs, e.g. Executive Director, does 100% get allocated to direct run services? Where would this be in the SCA model? Do you have to manually input 80% (if that is the percentage of direct run services provided by the CMH)? |
7/7/2021 | No, allocation is based on methodology developed by the SCA Workgroup, e.g. 80% direct run and 20% to non-encounterable cost center, or 80% to provider administration and 20% to managed care administration. Methodologies for allocating are outlined in the report and Excel template and they vary by cost center. Note that the allocation methodology is consistent with federal MLR requirements and definition of CMH employee and contracted providers. Allocation of business operations expenses is seen on the Non-Encounter CC Allocation tab of the SCA template, e.g. HR allocated based on FTEs in the cost center. SCA workgroup discussions agreed to standardized allocations, proportional to the use of the function, e.g. HR expenses benefit the CMH FTE. Noted that four categories of shared expenses are being considered for allocation to contracted providers for shared service, e.g. training, space, EHR, and fleet expense. See Q112 for further information. Please provide specific examples where it is perceived that there will be overallocation or under allocation to direct-run services for discussion at SCA workgroup. Updated SCA template will include sample data to show how the costs flow through the SCA model to illustrate how the allocation happens. |
| 114 | Managed Care Administration | Provider Network cost center does not who an allocation as it appears to be 100% managed care administration. Is that correct? One staff providing this work would have to split time into two cost centers, support for direct run providers and contracted providers. A similar question about Quality as CMHs and contracted providers do quality work. Is all managed care administration being shifted to the PIHP? |
7/7/2021 | Yes, provider network expenses are 100% managed care administration. The intent is for the SCA model not to be overly granular with a focus on consistency across CMHSPs. Please provide examples of quality related functions that should be considered provider administration for review at the SCA workgroup. Oversight of contracted network providers is considered managed care administration. The SCA model is designed to create consistency in definitions, e.g. CMH employee and contracted provider, and align with federal MLR regulations that do not allow layering of costs on top of the service cost paid to providers. |
| 115 | Non-Encounterable cost center clarifications / changes | Under cost center 210-Other Managed Care Administration, the example list includes ‘member surveys’. What is the definition of member? | 7/19/2021 | We use the term “member” in referencing a Medicaid beneficiary. The MACPAC definition is “A beneficiary is any individual who both qualifies for and utilizes the provided services and supports within Medicaid. Medicaid beneficiaries are often categorized by their eligibility status – financially, categorically, or medically needy. Children eligible for the Children's Health Insurance Program (CHIP) and aged, blind, disabled (ABD) adults are among the most common Medicaid beneficiaries.” For example, the MDHHS-PIHP contract requires PIHPs to provide to the State the mailing addresses, pre-survey and background information, and demographics needed to schedule and conduct the National Core Indicator (NCI) Surveys. If the PIHP delegated any of those functions to the CMHSP, the CMSHP would report that administrative time in cost center 210-other managed care administration. |
| 116 | Non-Encounterable cost center clarifications / changes | The definitions for cost centers: 201-Access and 202-Care Coordination are very similar. What are the defining differences? | 7/19/2021 | The “Access” function is related to Access Center activities of outreach, enrollment assistance, and provision of information to engage potential recipients, as defined in MDHHS Policy on Access System Standards. Care Coordination brings disciplines together to create, coordinate, and deliver an interdisciplinary, person-centered care plan for a recipient receiving services, and includes care management and coordination of services not encounterable as targeted case management. Care Coordination may include coordination of appointments, facilitation of engagement with needed services/providers, and communication with care providers for continuity of care. |
| 117 | Non-Encounterable cost center clarifications / changes | • The Quality department conducts training on navigation and an introduction to our Electronic Medical Record for any new clinical staff that are hired as well as conducts ongoing training for provider staffing. • The Quality department conducts training on Clinical Record documentation and documentation compliance for all new clinical staff as well as for ongoing training for current staff upon the request of supervisors. • The Quality department conducts record reviews of clinical records to ensure that clinical services are being provided appropriately and consults with the case manager and supervisor on corrective action if they are non-compliant. • The Quality department develops and creates reports and dashboards for data requested by supervisors and staff (these often include metrics for completion of documentation with consumers, outcomes monitoring and consumers being seen on a frequent basis). |
7/19/2021 | For the first example, different CMHs provide training by different staff, e.g. on the job, training department, or others. For training activities related to the Electronic Medical Records, this expense is categorized in the Medical Records cost center (216). Training activities generally would be placed in the 215 Training Net Expense cost center. For the third and fourth examples, if activities are directly related to quality improvement activities, e.g. if the chart reviews and dashboard are used to monitor and report quality improvement projects outcomes, the expenses fit into the Quality cost center (213) |
| 118 | Transportation | For our contracted providers, transportation is split out and paid separately. We have been adding in the transportation expense to the applicable service code when reporting total cost on the UNCs. There doesn’t appear to be any transportation codes in the FY22 code set. With not being able to add any additional costs into what is paid to providers, how would you suggest we report the transportation costs for FY22? Are there any transportation service codes that we can use? | 7/21/2021 | It is unclear whether the transportation in your question is performed by the contracted network provider or CMHSP. There are transportation codes in the SFY 2022 code sets along with a corresponding transportation cost center in the SCA methodology. MDHHS has set-up a pilot workgroup with volunteer CMHSPS to support unbundling transportation. This is not required, however, for SFY 2022. To the extent that you are providing transportation services as direct-run in SFY 2022 to support contracted network provider services, there are a two options: 1. The transportation service can become a direct-run service using the direct-run transportation cost center and submitted with a corresponding encounter to MDHHS 2. The SCA methodology outlines that the CMHSP direct-run transportation cost cannot be layered on top of contracted network provider services. The transportation cost would have to be included in what is paid to the provider. CMHSPs should then “chargeback” the cost of the transportation. This may not be an option in future years if transportation is no longer bundled, which will depend on MDHHS policy. There are several transportation codes in the FY22 code set including: - A0080 Non-emergency transportation services. - A0090 Non-emergency transportation services. - A0100 Non-emergency transportation services. (Taxi) - A0110 Non-emergency transportation services. (Bus) - A0120 Non-emergency transportation services. - A0130 Non-emergency transportation services. - A0140 Non-emergency transportation services. - A0425 Ambulance ground mileage - A0427 Ambulance ground mileage - S0209 Non-emergency transportation services - S0215 Non-emergency transportation services |
| 119 | Non-Encounterable cost center clarifications / changes | When needed, Interpretation expense has been a cost that we’ve added to various service codes, both direct-run and contractually provided. There is no service code for interpretation. How should we report the cost of interpretation for a contracted service? | 7/21/2021 | Costs associated with language interpretation services are administrative-related expenses, and should be assigned to the appropriate non-encounterable cost centers. |
| 120 | Service Cost Centers | For contracted residential services, codes H2016 & T1020, at times the consumer/individual is not in the home, in the past we’ve been able to add in the expense of those days as part of the overhead costs. Now that we’re not able to add any additional costs to the reportable HCPC codes, how will this be accounted for? How are others handling this? Are they estimating so many days out of the home and incorporating that into their per diem rates? | 7/21/2021 | CMHSP expenses should be assigned to standard expense categories and standard cost centers in accordance with the SCA instructions, which varies depending on the type of expense. For example, clinical salaries and wages attributable to the licensed residential cost center should be directly assigned to that cost center |
| 121 | General | Providers expect the CMHSP to pay them when someone is out of the home • Currently, they pay them for that day, but don’t report it as an encounter • Other CMHSPs add in a vacancy factor For residential codes, T1020 and H2016, did you say this afternoon that we are to allow providers to bill for every day regardless of whether or not face-to-face service was provided? So if the consumer is out of the home for a couple of days, the provider would still bill? |
7/21/2021 | The SCA does not alter the State's requirements for billing only for services actually rendered. The discussion regarding allocation of direct service staff salaries and wages for residential services is independent of what is allowed for provider billing purposes. |
| 122 | Allocation Clarifications | 1. Health insurance allocation – below is an example of what our health insurance expense would be per eligible employee if allocated by FTE vs Wages. The variance is significant between the pay grades and this would not reflect accurate costs for services. 2 CFR 200.431c says that benefits must be allocated in a manner consistent with the pattern of benefits attributable to the individuals or group(s) of employees, it doesn’t say you must allocated on the basis of wages. 2 CFR 200.431d says fringes may be allocated on wages, but such allocation is not to show a significant variance between groups. Please see 2 CFR 200.431 c & d below. If we allocate based on wages, it is a significant variance between groups and this is not allowed. What other option do we have to allocate? Example by pay grade was provided. (c) Fringe benefits. The cost of fringe benefits in the form of employer contributions or expenses for social security; employee life, health, unemployment, and worker's compensation insurance (except as indicated in § 200.447); pension plan costs (see paragraph (i) of this section); and other similar benefits are allowable, provided such benefits are granted under established written policies. Such benefits, must be allocated to Federal awards and all other activities in a manner consistent with the pattern of benefits attributable to the individuals or group(s) of employees whose salaries and wages are chargeable to such Federal awards and other activities, and charged as direct or indirect costs in accordance with the non-Federal entity's accounting practices. (d) Fringe benefits may be assigned to cost objectives by identifying specific benefits to specific individual employees or by allocating on the basis of entity-wide salaries and wages of the employees receiving the benefits. When the allocation method is used, separate allocations must be made to selective groupings of employees, unless the non-Federal entity demonstrates that costs in relationship to salaries and wages do not differ significantly for different groups of employees. |
8/4/2021 | The SCA Workgroup discussed this issue and it was determined to not be a statewide issue. Instead, this may require individual CMHSP technical assistance. Please also see the response to question number 92. |
| 123 | Service Cost Centers | Please explain what you mean by joining these 3 together on Appendix 2 in a Std Cost Center Code with specific HCPCS codes. Does it mean they are interchangeable so we can lump all HCPCS codes listed under "112/117/118" with either 112, 117 or 118. or can we mix and match? Some of those codes with 112 and some with 117 as we deem appropriate? |
8/4/2021 | The HCPCS listed in the “112/117/118” are not assignable to other cost centers deemed appropriate by the CMHSP. Instead, the HCPCS codes listed under “112/117/118” have a mixture of types of providers which each fall into different cost centers. For example, 90832, has qualified providers of psychiatrist, physician, and registered nurse – all of which are in the psychiatric services – medical clinic cost center; and psychologist, Master’s level social worker, licensed professional counselor, marriage and family therapist, Master’s level in Human Services field, and Bachelor’s level in Human Services field – all of which are in the outpatient cost center. The goal of having a single HCPCS code going to multiple cost centers was to reduce the number of cost centers staff would need to track. Please see response to question number 32. |
| 124 | Service Cost Centers | Cost Center 206 is for administration costs associated with Grants ( and non clinical contracts). What cost center is used for the direct expenses associated with these? Do all costs (wages, fringes, etc.) go in under 206? It is extremely misleading to call Grants the "Unique administration supporting other non-Medicaid/GF activities". As an example, we have a contract with the Montcalm Area Intermediate School District to provide Masters Level Social Workers to work in the school districts in the County. They use the MAISD reporting system for the services they provide, we receive no encounter data. These staff are full time employees of MCN and receive clinical supervision from MCN staff and we would also need to allocate the 3 fringe benefit expense accounts, all based upon wages of staff in the cost center. Also Finance, General Administration, HR and IT administration cost centers would also be allocated to this contract. From what I can tell on the Non-Encounter CC Summ the only Salaries and Wages picked up is for wages expense code 06, so the wages would go here because they do not fit any of the other 5 wage expense categories. |
8/4/2021 | Salaries should be directly assigned based on the SCA instructions to the appropriate standard expense category and then assigned to clinical and non-encounterable cost centers. Salaries for employees supporting grants would assigned to 206, Grants. Employee benefits and other fringes are allocated proportionately through the SCA template based on the salaries and wages assiged to each of the cost centers. We will discuss with the SCA Workgroup revising the administrative cost category name "Unique administration supporting other non-Medicaid/GF activities" to be more clear that this is Non-encounterable Grant expenses. This was originally developed broadly and we agree that it could be revised for clarity given the Grant cost center is the only one being assigned. |
| 125 | Service Cost Centers | Per the methodology, Recipient Rights is charged to cost center 209 - Mental Health Code/CMHSP Only Activities, along with a lot of other activities that are mostly GF funded. As was found out in the EQI submission for FY 2020 most of Recipient Rights costs are funded by Medicaid and Healthy Michigan, not GF. I see no "method" in the SCA to determine how cost center 209 is allocated by funding source. Is there a plan to do this, or are we to determine that "off" SCA? | 8/4/2021 | The SCA template has been modified to include an "Administrative Cost Summary" tab which shows the allocation of expenditures by population and fund source. This table is driven by the CMHSP direct-run minutes by code, population, and fund source on the "Service UNC" tab. This table and other updates will be available in the newest version of the SCA model. |
| 126 | Expense category strategy | In assigning costs to activities of the 6 "all other managed care administration" and 2 "healthcare quality improvement activities" categories, how accurate do we need to be. If it is too difficult to split an activity between multiple categories, can we pick the most appropriate to put it in? In the PHIP and CMHSP Standard Cost Allocation Methodology, Revised Draft 7/6/21, each had a description of what they are comprised of. We would use this as the basis. | 8/4/2021 | We have discussed the issue of materiality for accounting of activities, with a 5% threshold, so if the time spent is minimal, no separate tracking is required. If a position splits their time between cost categories, you would account for the time in the two categories. In particular, quality improvement activities are required to be accounted for separately as they are a component of the MLR calculation. |
| 127 | Allocation Clarifications | I’m trying to determine the best way to ensure that our GL reconciles to the SCA, EQI & FSR. To do so, it may be easiest to complete the admin allocations in our GL before entering the trial balance into the SCA Report/Tool. I want to clarify that you want the admin allocations done not only by cost center but by the 20 standard expense categories as well. It appears from the SCA Report/Tool worksheet that you want to be able to summarize all expenses by the 20 standard expense categories, which means we would need to allocate admin cost centers by these categories. This will substantially increase the number of allocations that will need to be done monthly. Another significant issue is reconciling the fund source from our GL to the SCA, EQI & FSR. We need to know where our spending by fund source stands at all times. The SCA/EQI allocates to fund source by direct run minutes. Has anyone on the workgroup come up with a process to reconcile their GL fund source to the SCA/EQI? |
8/4/2021 | Yes, the expenses should be allocated by cost center and expense category. One of the objectives of the SCA methodology is to retain the detail related to the type of expenses being allocated to see what is comprising the costs. Regarding the question on fund source, please see the response to question number 128. |
| 128 | Service Cost Centers | In our Case Management Cost Center, we provide T1017 services to other CMHSP's and bill them under COFR. These services are not reported as encounters by us to our PHIP. The services are reported by the receiving CMHSP. The cost center is allocated by funding source based upon the minutes of direct service billed as encounters. Currently we deduct what we bill to other CMHSP's from the total cost center costs and use that as the cost to distribute by funding source, and do not have to worry about breaking this deduction down by 12 expense account codes. How do we reflect this on the SCA? Because we are billing the other CMHSP's a predetermined fee-for- service rate, the actual cost rate calculated on the EQI report would be different. In addition, there are no "encounters" for the EQI for this funding source. |
8/18/2021 | SCA Workgroup discussed this question and agreed to include a COFR revenue column on the final direct run cost center summary tab. The assumption is that expenses are equal to revenues and any differences will be spread across all other services within that cost center. |
| 129 | Service Cost Centers | How should a CMH encounter report (what code/modifier) and track costs (what cost center) for Peer Services when the employee has been trained but before they have been certified? | 8/18/2021 | MDHHS is in agreement that Peer Services performed by a non-certified peer should be billed under H0038 with an HM modifier. |
| 130 | Allocation Clarifications | The following list a few things that need to be considered for the SCA Model: Expense categories a. Other employee benefits – finding instances of things that are not salaries/wages, taxes, insurance, or retirement related (i.e. tuition reimbursement, gym memberships, etc.) b. Revenue Offset – should be a negative number and represents situations where revenue received is treated as an offset to expenses before cost allocation occurs c. Other expenses – I think this category needs to be allowed in DR clinical cost centers also d. Salaries and Wages – Service Support Staff – realizing this needs to be Direct Allocation not Direct Assignment. Cost Centers a. Allocated – should be an option for CMHs who choose to aggregate costs in a cost center before directly allocating (i.e. Vehicle Fleet Cost Center, Services Support Staff Cost Center, etc.) |
8/18/2021 | Initial responses to these items will be discussed at this Friday's SCA Workgroup meeting. Expense categories a. Other employee benefits – we would propose to rename and include other fringes in Expense Category 09 (Pension and Retirement Expenses), which is allocated based on salaries and wages. b. Revenue Offset – the next update to the SCA model will include data validation to ensure that offsets are entered as negative numbers. c. Other expenses – can you please provide examples of other expenses that should be directly assigned to direct-run clinical cost centers? If other expenses are allowed, the SCA Workgroup should consider developing a list of Other Expenses that could/should be directly assigned. d. Salaries and Wages – Service Support Staff – for SCA Workgroup discussion on 8/20 Cost Centers a. Allocated – for SCA Workgroup discussion on 8/20 |
| 131 | CCBHC | In response to the request for detailed feedback on what is not included in the SCA Model that is included in the CCBHC Cost Report: 1) Standard Cost Allocation (SCA) does not treat DCOs correctly in terms of indirect and admin costs incurred by the CCBHC on behalf of the DCOs. Currently SCA is putting DCOs in contractual services and therefore the indirect/admin is treated as managed care. The CMS CCBHC cost report includes the DCO costs as a direct service cost in the indirect cost calculation which in turn is part of the PPS-1 rate calculation. 2) Standard Cost Allocation does not give the CCBHC the option to elect the 10% de minimis for indirect costs, which is a legitimate and valuable option that CCBHCs may wish to elect (such as Macomb). |
8/18/2021 | For MDHHS discussion and SCA Workgroup discussion on 8/20 |
| 132 | Allocation Clarifications | Where do you anticipate space costs would be accumulated before allocating to other cost centers? You have expense code 17 "Facility and Equipment-Related Expenses" for these costs. Are these expected to be allocated outside of the SCA, with the resulting summary allocation entered into the SCA? You removed the property cost center you initially created ( which is where I would expect to put these costs) per Q&A #111 which state we are to put thesein costs center #403. This does not make sense to me because #403 is a dead end account that is not further allocated. Currently we have several buildings that each have their own cost center, where the users of that building are allocated that buildings costs. Given your basic theory for the SCA I would assume we put all of these facility costs together and allocate the total among the direct run and 200 and 300 series cost centers. If so, where do I accumulate my space-related costs? I have rent, utilities, equipment purchases, building maintenance staff wages and fringes and depreciation. |
8/18/2021 | For SCA Workgroup discussion on 8/20 |
| 133 | Allocation Clarifications | Vehicle, other and wages paid to recipients - direct assignment. Refer to examples in Appendix 1, e.g. office supplies. Wages paid are separated out as non-allowable in clinical or Medicaid costs, exclusive of supportive employment program. Circle back and clarify/guidance on treatment of supportive employment. | 4/23/2021; Updated 7/7/2021 | Additional information has been provided in Appendix 1 and 2 regarding wages paid to individuals receiving services. |
| 134 | Allocation Clarifications | We currently have staff that have higher wages that are part-time that do not qualify for insurance. This will skew our costs when looking at an actual program for sustainability. Our approach is to allocate based on actual staff with insurance. | 6/10/2021; Updated on 7/7/2021 | The SCA approach is to allocate based on salaries and wages. This is a whole cost allocation process. The SCA Workgroup will review after SFY 2022 reporting and determine whether this approach was materially different than if directly assigned insurance costs to employee or eligible employees. The selected approach seeks to find a balance between consistency, materiality, and administrative burden. This creates a more consistent approach. We also did not want to jeopardize allocations in alignment with 2 CFR 200 and do not see results as materially different. |
| 135 | Service Cost Centers | According to the Service UNC tab of the most recent draft with examples, H0050 is proposed to be under either Psychiatric Services - Med Clinic or Outpatient cost centers. Shouldn’t it fall under the Case Management cost center instead as it is a brief intervention for alcohol/other drug treatment service? | 9/1/2021 | H0050 is 15-minutes of an SUD program and is used for case management as well as other services to support treatment plans/goals and is appropriate for the Outpatient cost center. This can be provided by a multidisciplinary team, case manager, or SUD clinician (must be a practitioner). Three case manager codes are used for Medicaid delivery of service as part of an SUD developed treatment plan goals: H2035 - hour H2036 - per diem H0050 - per 15 minutes H0050: Alcohol and/or drug treatment program, per 15 minutes – is 15 minutes of outpatient alcohol/or other drug treatment service in which the client participates in accordance with an approved individualized treatment plan that includes culturally relevant activities, as appropriate. It may include assessment, individual and group counseling, occupational therapy, activity therapies, expressive therapies (art, drama poetry, music, and movements), referral and information, drug screening urinalysis, medication administration, medical services, case management services, and nutrition counseling. T1017 (Targeted Case Management, each 15 mins) is not appropriate for targeted SUD case management. H0006 (SUD Case Management) is not a Medicaid or HMP-covered service in Michigan. If Medicaid is not involved as a payer (Block Grant), then H0006 is the code to utilize for SUD case management: |
| 136 | Allocation Clarifications | Per the definition of the cost centers, Recipient Rights costs are accumulated under cc 209 - Mental Health Code/CMHSP Only Activities, and summarized in the "Non-Encounter CC Summ" worksheet with the final total in column V of that worksheet (e.g. $120,000). From there it appears on "Non-Encounter CC Allocation" in the row for cc 209 in column F. In this work sheet to this amount is allocated: Finance, General Administration, HR, IT, Trainers Net Expense, Supervision and Medical Records if applicable. The total after these allocations is in column T (e.g. now it increased $135,000). The description in red beside it in column C is " Unique non-encounterable CMHSP only activities(e.g. MHC)" . From there it goes to the Administrative Cost Category schedule Excluded Services - Unique non-encounterable CMHSP only activities (e.g., MHC)" in cell C10 on the "Administrative Cost Summary" worksheet. What happens after this? Is this the final stop and it is considered 100% GF administrative cost? Currently we allocate 95% of this amount to Medicaid as most of the consumer rights workers activities surround services received by Medicaid eligible individuals. If this is the final resting place of recipient rights costs, in FY 2022 our GF expense for this would end up being about $121,500 ($135,000 times 90% GF matching funds share), which alone would be 12.2% of our $997,046 GF authorization for FY 2022. The method we are using in FY 2021, which would assign most of this Cost to Medicaid, would result in a GF amount of about $6,000 ( $135,000 times 5% GF time 90% GF matching funds) would only be about $7,000. Would this be a reconciling adjustment on the EQI report? If so, this is going to be a big complicated mess because this will not be the only reconciling adjustment. This further complicates trying to be able to develop an internal cost allocation plan to match the activities in our General Ledger to the processes in the SCA. |
9/15/2021 | The Unique non-encounterable CMHSP only activities (e.g., MHC) are included on the Administrative Cost Summary tab. We will be modifying the non-benefit expense tab of the EQI to include rows attributable to this cost center and have done so already within this tab. It is assigned to Medicaid and General Fund services based on direct-run and contracted network provider expenditures from the Service UNC tab. |
| 137 | Allocation Clarifications | From what I can tell so far, the SCA does not allow for the accumulation in a specific cost center within the SCA for each of the three categories for fringes. This requires each to be allocated outside of the SCA and then entered in the "Standard Summarized TB" tab. For example, 08 Insurance expenses - Health Insurnace. We pay about $110,000 per month for health insurance. Without first allocating this amount to cost centers based upon wages by cost center and then entering the resulting amounts, I have no place to put the $110,000 along with all other insurances that are booked to expense 08. What I am stating is that although the SCA will allocate the three fringe benefit accounts based upon cumulative wages, you first have to internally calculate that allocation in your General Ledger before you can enter the various fringe benefits that make up the three SCA fringe benefit expenses. I am trying to match my General Ledger activity to what goes on in the SCA workbook. Having to do this internally helps me to be in cinq with the SCA. If I do not use internally the same allocation method as the SCA workbook, this of course will cause a discrepancy. What is not so easy to cinq is what the SCA does with 200 series cost centers. This will require a complete reconstruction of activities into the defined accounts. The only cost center that will survive intact will be Human Resources. |
9/15/2021 | The updated version of the SCA model included Direct Allocation cost centers that allow for pooling of the fringe expense category expenditures. |
| 138 | General | I cannot find where the amounts shown in Column I "Provider Admin" on the "Final DRClinical CC Summ" are calculated. The total of this column is the source for the amount shown on the "Adminisrative Cost Summary" in cell C20 - Direct-Run Clinical Provider Administration. | 9/15/2021 | These amounts are the sum of all provider administration pieces from the "Initial DR Clinical CC Summ", "Expense Category Allocation", and "Non-Encounter CC Allocation" tabs. Each of the 3 tabs listed contains cells with red text at the bottom of the tables indicating which categories fall under provider administration. The same can be said for the other categories (Direct Staff Salaries and Wages, Employee Related Expenses, etc.) |
| 139 | Expense category strategy | At the Aug 18th a question was asked about where to expense fringes that are neither employment tax, insurance nor pension. This would be all other fringes such as tuition/student loan payments and health club dues. Months ago we were told to charge these to the HR cost center where they would be allocated with the HR costs. Your response on Aug. 18 was that we could include them as pension expense. Will this be added to the Appendix 1 under the definition of Expense Code 09 - Pension and Retirement Expenses? |
9/15/2021 | Line 63 has a similar question regarding EAP and other employee wellness functions that are HR functions and an HR expense. A gym/health club membership would more appropriately align with fringe benefit expenses and should be reported as such. The updated SCA methodology includes other fringes with the Employee Insurance expense category. |
| 140 | Expense category strategy | In what cost center would costs go that are 100% local obligation? These include: Local Match Contribution Local Share of State Facility costs ( State pays directly the state share, we are only billed for the Local share and pay it is a local cost only) Non-matchable expenses In Montcalm Care Network's case this amounts to about $400,000 in the current Fiscal Year. If they are part of cost center 209, we would have to break out separtely for futher reconciliation to FSR. The beauty of having an all-inclusive SCA is that everything is in one place. This is why the CMHSP has to maintain its' own all-inclusive cost allocation worksheet to calculate many things that are not possible within the SCA, yet still has to following the SCA method with-in its' own cost allocation worksheet to have any hope of reconciling the SCA to the FSR. |
9/15/2021 | This will be discussed during the next SCA Workgroup meeting. |
| 141 | Service Cost Centers | HCPSC for grants in encounterable cost centers: The SCA Model groups T1017 in Case Management: codes 90832,90834, 90837 and H0032 in Outpatient, and H0038 in Peer Supports. We have grants that pay for the salaries and wages of staff working in our County Jail. During the course of their work the staff record the above HCPCS codes as well as an indirect code for services they provide that do not fit one of the HCPCS codes. Knowing what I knew up to this point about the SCA, I was going to record the expenses of these staff, including the amounts not reimbursed by the grant ( such as supervision, IT and administration) in cost center 206 - Grants. However, strictly following the SCA model, if these HCPCS codes have to go under the appropriate cost center, how do I get the costs into the Outpatient, Case Management and Peer Supports cost centers to build up the costs for these services and do they count as GF or Grant funded? In the past these services were never submitted to the PHIP and therefore were considered non-encounterable. They were set up in the Electronic Health Record (PCE) in cost centers that, based upon the parameters set for the cost center, did not consider these encounterable services and they were not submitted to the PIHP as such. In FY 2020 there were approximately 400 encounters performed. I can only count the service once. What I would like to do is go "off" the SCA, keep the cost centers I have used, not include them in reporting costs and services for the standard SCA encounterable services, record the costs as cost center 206. However, the costs would be split by the grant (wages and fringes for direct staff) to cost center 206 and GF only ( the rest of the expenses) to cost center 209. Splitting GF and Grant Cost Centers: In the SCA model there is no way to split costs between cost center 206 and 209 in the above-mentioned grant situation. Since the grant is only paying for wages and fringe benefits, if I charge those to cost center 206 (Grant), and the direct expenses cost center 209 ( Mental Health Code/CMHSP Only), the wages and fringe benefits will be used to allocate expenses that are not reimbursed by the grant, such as supervision, space, other expenses, and administration, to cost center 206. How do I get the expenses to follow the funding source? |
9/15/2021 | The SCA Workgroup discussed this topic during our last call and is proposing that all encounters related to HCPCS codes should be submitted to the PIHP and then to the MDHHS data warehouse. Therefore, individuals performing these encounterable services should continue to report their time in the appropriate clinical cost center as opposed to the Grants cost center. The total Grant expenses, as an example, will equal the total expenses allocated to the Unique non-encounterable Grant activities administrative cost category (included on the Administrative Cost Summary tab) plus the expenses on the Service UNC attributable to encounterable services. Please provide any feedback you have related to the proposal that all encounters related to HCPCS codes should be submitted to the PIHP and then to the MDHHS data warehouse to Kathy Haines as this issue impacts many MDHHS initiatives. |
| 142 | Grants | From Q&A Session: Topic Grants: what about staff who are directly allocated to grants for direct delivery of non-medicaid services? What is the expense category? Would that work to split a grant and GF split paying for a grant? If services are fully grant and no state funds being used, why would we have to send an encounter and report to the State at all? Do other providers have to do that? |
9/15/2021 | Grant services salaries and wages would go under cost center 206/Grants directly assigned, not allocated. Expense category is 06 Salaries and Wages, Administration or 01 Clinical Direct Services staff if encounter related. The Coordination of Benefits (COB) group is working on how to handle grant and GF. If an encounterable service is not fully covered by a Grant, the Grant would act like a COB. Please also see response to question 141. |
| 143 | Medical Records | From Q&A Session: Medical Records: We account for our EMR as an IT cost. What costs are you expecting to see in Medical Records? So the EMR is 100% EMR? Clinical staff use EMR to record billable services that is EMR Med Records? |
9/15/2021 | Types of expenses include any chart supplies, release of records, or other medical records related expenses. The system expenses are in IT; EMR expenses are as noted above. Clinical staff charting is indirect time of direct care provision. |
| 144 | Expense category strategy | I have questions concerning what expense category and cost center to use for the following: 1.) Payment to MDHHS for the local share of state facility costs. This is 100% local. 2.) Payment to our PIHP for the local match draw down amount. This is 100% local. 3.) Payment of a donation that is not chargeable to Medicaid or GF. This is 100% local. 4.) Payment to MDHHS for the cost of a DSS staff person to be on sight to answer and resolve Medicaid coverage. This a 90/10 split between GF and local. |
9/15/2021 | This will be discussed during the next SCA Workgroup meeting. |
| 145 | Allocation Clarifications | What is the purpose of darkening some of the cells on the "Non-Encounter CC Summ" tab? For example, columns E,J, K, P, Q, are mostly darkened, but all cells in each have formulas? Is the purpose if there is a number in one of those cells, you made an error? It shouldn't be, because payroll taxes, Insurance and other fringes, Pension and Retirement, Facilities and Vehicles would be an appropriated allocation to the cost centers listed. | 9/15/2021 | The columns that are darkened are those in which the expense category is directly assigned. The columns in which the dollars for the expense category are allocated are not darkened. Please notice that when the drop-down options on the "Expense Category Summary" tab in column E are set to "Direct", the columns in question are no longer darkened. The formulas remain as conditional if statements for expense categories that can be directly assigned or allocated. |
| 146 | Service Cost Centers | Under expense category 10 - Network Provider Services, Clinical, it lists examples as: Clinical services contracted with other CMHSP's Clinical services contracted with community providers Does this mean we are to put all of the contracted provider service costs here, broken down by the Direct Run cost centers? There is no other type of cost that would go here. Since the breakdown by fund source and CPT code will not be in the SCA, and this amount does not go any further in SCA, is it optional to put any amount here? Or, we could just put the total amount of contracted services here in one cost center so that our total expenses are initially entered some place on the SCA. |
9/15/2021 | The SCA methodology is primarily intended to allocate costs incurred by CMHSPs to either direct run clinical services or to administrative functions. Contracted network provider services do not have any cost center requirements, but can utilize the existing cost centers if a CMHSP opts to do so. The contracted network provider service costs and units should be directly assigned based on the service codes actually billed for and paid by the CMHSP. Appendix 2 provides a complete list of the direct-run clinical cost centers and the corresponding CPT codes that should be used to map expenditures to each cost center. |
| 147 | Allocation Clarifications | Same question as on the Non-Encounter CC Summ. It is clear that in columns R,S, T, U,V,X and Y that the darken rows are in the cost centers being allocated to other cost centers so they are darkened. But if they are not supposed to be, why is there still a formula in those cells? As to Colum W for Supervision and Column Y Salaries and Wages, Service Support Staff for Allocation, why are they open to allocation formulas for the non-direct run cost centers? Could you make it clearer on the work sheet which base is being used to allocate the non-encounterable cost center allocation amounts for each cost center? What is the purpose of the DR FTE (Column K) and the DR-Clinical Salaries and Wages (Column L), what is being allocated on these basis? |
9/15/2021 | We have zero'd out the formulas in columns D through I for the grey shaded cost centers (i.e. those being allocated across all other cost centers). We can remove the formulas in columns R through Y given that is causing confusion. We can remove formulas for Supervision and Service Support staff in the non-encounterable cost center rows to avoid confusion. Row 1 in columns R through Y identify the allocation basis. The purpose of the DR FTE and DR-Clinical Salaries and Wages columns are for allocation of Trainers Net Expense (Column V) and Supervision (Column W). |
| 148 | Allocation Clarifications | I am currently working on putting test data into the SCA template and I am stuck on the cost allocation for Standard Expense Category 08 and 09. We are using “Direct” for both but the cost is showing in the “Expense Category Allocation” column in addition to the other two cost columns (H and I). Should the cost be showing in column J “Expense Category Allocation”? | 9/15/2021 | This was determined to be a formula error in the most recent version of the SCA model. We will be providing an updated model with conditional formulas to ensure that when "Direct" is selected that it does not also use the "Expense Category Allocation". |
| 149 | Allocation Clarifications | For Standard Expense Category 17 it no longer gives me the option to select Square feet as an allocation method. | 9/15/2021 | With the addition of other expense categories that can be directly allocated over various allocation bases, the model now simply has options for "Direct" or "Direct Allocation". Selecting "Direct Allocation" for the Facility and Equipment-Related Expenses expense category will allocate those expenses by square footage. |
| 150 | General | What are all the due dates for this for SFY 2022? | 9/15/2021 | The SCA reporting will coincide with the EQI reporting. MDHHS will provide the EQI timelines for SFY 2022 as soon as possible. |
| 151 | General | Will each submission show stand alone costs, or is it cumulative? | 9/15/2021 | Each successive reporting period during the year will be cumulative. For example, the Period 2 report will reflect the first 8 months of the year. |
| 152 | Service Cost Centers | Will transportation codes T2003 and S0215 be added to the Appendix 2 under cost center 125? | 9/29/2021 | T2003 and S0215 have been added to the transportation cost center along with other updates in the newest version of Appendix 2. |
| 153 | Service Cost Centers | How do you code an independent facilitator, facilitating a person centered plan, for a consumer that is only case management or not outpatient. The facilitation code, H0032, only shows up in Appendix 2 as cost centers: 112/117/118. Should it be included in cost center 104 | 9/29/2021 | An independent facilitator would use the modifier WQ. The provider qualifications list this code as "treatment planning" and description of "Mental health service plan development by non-physician" so it is developing "person centered planning". The state said they want to track the case management activities, so it makes sense that treatment planning is part of coordinating care and could use CC 104. H0032 with modifier WQ has been added to CC 104 in the newest version of Appendix 2. |
| 154 | Other | On the website under the Policy 2077 Documents tab there is a "Mental Health & Substance Use Disorder Reporting Requirements" section. Is this now where SCA information will be posted? | 9/29/2021 | The SCA model, instructions, methodology, and appendices will all be posted under the Policy 2077 Documents tab in the "Standard Cost Allocaton Methodology" section. |
| 155 | Other | On the provider cost tool reporting for those over $1m, the concern is that contract providers will not know the funding source being used to reimburse them, and may not group their cost centers, expenses, and time and attendance in alignment with the model. | 9/29/2021 | The level of detail being requested from contracted network providers is not as detailed as the CMHSPs and is not anticipated to require changes to the provider chart of accounts to complete the request. It is optional to report cost centers consistent with the SCA methodology. Request that providers submit feedback. Noted that providers not knowing the funding source is reasonable and we will consider possible adjustments to the template. |
no reviews yet
Please Login to review.