221x Filetype PDF File size 0.78 MB Source: cdn.ps.emap.com
Copyright EMAP Publishing 2017
This article is not for distribution
Nursing Practice Keywords Nutrition/Protected
Practical procedures mealtimes/Malnutrition/Documentation
Nutrition and hydration This article has been
double-blind peer reviewed
Assisting patients with eating and
drinking to prevent malnutrition
alnutrition costs the UK This is essential as it helps to ascertain
Author Liz Anderson is nutrition health economy £19bn a year whether a patient needs help and informs
nurse specialist at Buckinghamshire and affects one in four people their nutritional plan of care.
Healthcare Trust. M
admitted to care settings There are a number of patients who
-
(Elia, 2015). It is most prevalent in the com have medical conditions that mean that
Citation Anderson L (2017) Assisting munity but nutritional status often deteri- they may need assistance with eating and
patients with eating and drinking to orates when patients are admitted to hos- drinking; these are summarised in Box 1.
prevent malnutrition. Nursing Times pital because of acute injury or illness that
[online]; 113, 11, 23-25. Preparing for mealtimes
can impair swallowing, appetite and
gastric absorption. When patients are Nurses should assist patients to make
unwell and do not feel like eating it can be a appropriate meal choices; for example, if
- -
Box 1. Medical conditions challenge to help them meet their nutri they can only eat soft food due to poor denti
that may affect eating and tional needs. tion they should be made aware which foods
drinking Patients with malnutrition will have a on the menu are soft and easy to chew.
deficit of vitamins, protein, minerals and Nurses should not choose food for patients
Swallowing complications: may be energy and this will have an adverse effect without consultation; if they are unable to
associated with conditions such as on the body. Complications associated choose for themselves, their nurse should
stroke, Parkinson’s disease, motor with malnutrition include poor wound speak to a carer or relative to find out their
neurone disease and multiple sclerosis healing, skin breakdown, increased risk of likes and dislikes where possible.
sepsis and hospital-acquired infections, As part of the assessment process, it is
Cancer: some patients with cancer have such as chest and urinary tract infections important to know whether patients have
increased energy requirements but they
(Elia and Russell, 2009). Provision of any special dietary needs. For example, a
may feel unable to eat due to nausea, adequate nutrition and hydration is a patient who has swallowing difficulties
vomiting, pain or gastrointestinal hallmark of good, compassionate care but (dysphagia) may need a texture modified
obstruction. Patients prescribed -
remains neglected in many areas of health diet (National Patient Safety Agency, 2011)
chemotherapy often experience a care (Leach et al, 2013). as giving food that is difficult to swallow
change in taste which can affect
The Hospital Food Standards Panel may lead to choking. This information
their appetite report (Department of Health, 2014) rec- should be obtained when admitting the
ommends that all NHS hospitals adhere to patient to hospital and shared with the
- -
Surgery: people who have had surgery and be compliant with the Ten Key Charac multidisciplinary team; refer to local poli
require extra energy to help heal teristics of Good Nutritional Care (Council of cies for further guidance.
wounds but they can sometimes find Europe, 2003); this includes ensuring an
eating difficult due to pain and nausea environment that is conducive to patients Protected mealtimes
-
being able to enjoy their meals uninter It is best practice for clinical areas to follow
Other: people with severe learning rupted. Good nutrition and hydration is a protected mealtime policy. During pro-
disabilities, visual impairment or part of the Care Quality Commission’s tected mealtimes, all non-urgent clinical
dementia, and older people who have Fundamental Standards (CQC, 2015) and activity should stop and staff should take
an acute delirium, need specialist all care settings are expected to demon- the time to help patients to eat and drink in
support to ensure they are adequately strate how they put nutrition and hydra- a relaxed, and unhurried atmosphere
nourished tion at the heart of patient care. (Council of Europe, 2003).
It is essential that all patients receive While this can often be challenging in
adequate food and drink appropriate to practice, especially in a busy acute envi-
their needs (Nursing and Midwifery ronment, staff should make every effort to
Council, 2015) and while many will be able ensure that patients are able to eat and
to manage independently, some patients drink their meals without unnecessary
will need assistance. interruptions.
All patients admitted to care settings Many organisations encourage family
- and carers to come in at mealtimes to assist
should have nutritional screening per
formed within the first 24 hours (CQC, their relative with eating and drinking.
2015; National Institute for Health and This is good practice, particularly for
Care Excellence, 2006) using a validated patients with dementia or learning disabil-
tool such as the Malnutrition Universal ities as they may be more willing to accept
Screening Tool (MUST) (Bit.ly/MUSTtool). help from a person they know.
Nursing Times [online] November 2017 / Vol 113 Issue 11 23 www.nursingtimes.net
Copyright EMAP Publishing 2017
This article is not for distribution
Nursing Practice
Practical procedures
Fig 1a. Red tableware can highlight people who need help risk of cross infection and put on an apron
(Dougherty and Lister, 2015).
3. Assist the patient to sit in an upright
position at a table in a dining room, in a
chair by the bed or upright in bed if the
patient cannot get up. This helps with swal-
lowing and protects the airway (Dougherty
and Lister, 2015). Eating in a dining room
also makes the meal a social occasion.
4. If the patient use dentures ensure they
are clean and offer assistance to insert
Fig 1b. Adapted cutlery helps those with restricted movement them if necessary.
5. If necessary decontaminate your hands
before handing food and allow the patient
to wash and dry their hands before the meal.
-
6. Protect the patient’s clothing with a ser
Right-hand Left-hand viette to maintain dignity.
spoon spoon
7. Sit down at the patient’s eye level. This
aids effective communication but also pro-
vides reassurance the patient that you have
the time to help the patient to eat (Fig 1c).
8. Do not be distracted by what is going on
around you or talk to other people.
9. Tell the patient what is on the plate – this
is particularly important for those who are
are visually impaired or eating a puree diet
Knife as food may not be instantly recognisable.
10. Ask whether the patient wants any
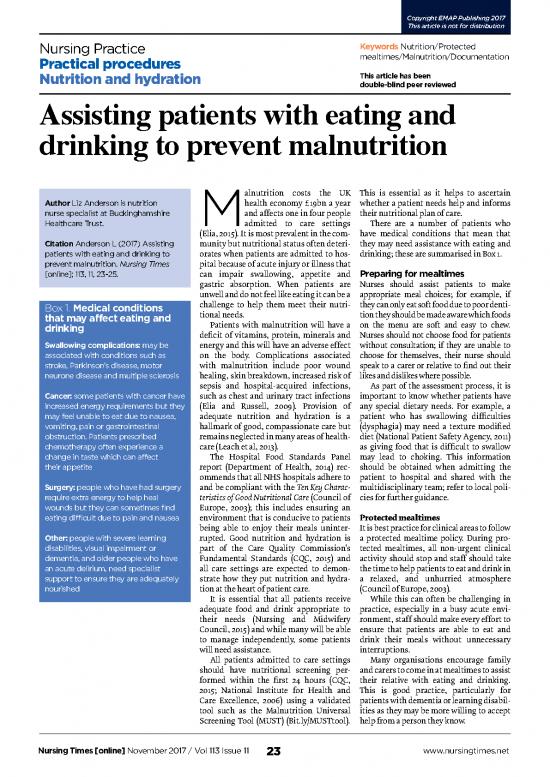
Equipment assessment what help the patient needs, for example: seasoning or sauces and has a preferred
The use of red tableware such as red trays, l Unwrapping packets; order in which they wish to eat the food.
jugs and beakers can help to highlight l R emoving yoghurt pot lids;
patients who need help with eating and l Cutting food into bite size pieces to 11. Ask how the patient would like to
drinking. This assessment should ideally promote independence. receive the food; some may prefer a fork,
be made at the same time as the nutritional others a spoon. It is important to let the
screening and included as part of their care Assisting patients patient feel in control of the mealtime.
plan (Fig 1a). This is an ongoing process Helping patients who cannot eat and drink
and should be reviewed regularly. independently takes time, understanding 12. Visually impaired patients should be
Adapted cutlery such as easy-grip han- and patience. It must not be rushed and told what you are putting on the fork or
dles and other equipment such as plate any nurse who is involved in this task
guards and nonslip mats can be useful for should not be interrupted. Box 2. Preparation checklist
patients who have restricted use of their
hands or who have had a stroke and can Equipment l Is the bedside table clear of clutter
only manage to eat with one hand (Fig 1b). l Clean table or tray; and of the right height for your
- l Ga ther equipment required to assist the patient to eat comfortably?
These are usually provided by an occupa
tional therapist. patient to eat, such as adapted cutlery; l Has the patient been given the
l Provide a serviette to protect clothing; opportunity to use the toilet and
Preparation for mealtime l Obtain a chair to sit beside or opposite wash their hands?
Before mealtime, nurses should ensure all the patient (Dougherty and Lister, 2015). l Does the patient have dentures in
patients are prepared to eat their meal in a and hearing/visual aids on if worn?
dining room or in a chair by their bed. If The procedure l Does the patient have all necessary
this is not possible they should be sat up in 1. Explain to the patient that you are going items within easy reach?
l Once the meal has been delivered,
amb bed, well-supported with pillows (see to help them to eat their meal.
L checklist in Box 2). Independence should is it what the patient ordered?
peter be encouraged and it is important to assess 2. Decontaminate your hands to reduce the
Nursing Times [online] November 2017 / Vol 113 Issue 11 24 www.nursingtimes.net
Copyright EMAP Publishing 2017
This article is not for distribution
Nursing Practice
Practical procedures
spoon before raising it to their lips. Do not Fig 1c. Sitting with your patient at eye level helps with
overload the fork. Bring it up to the communication and reassures them you have time to help
patient’s mouth to avoid the need to bend
to reach the food. Allow plenty of time for
the patient to chew and swallow.
13. When patients have a small appetite,
suggest that they try to eat a little of each
course for a balanced nutritional intake.
However, these patients are at high risk of
malnutrition and should be referred to a
dietitian to assess their dietary intake.
14. Offer sips of fluid after every couple of
mouthfuls; this can help eating.
15. When the patient has had enough of the Box 3. How to complete a food/fluid chart accurately
main course, offer dessert in the same way.
Make sure the spoon is the correct size, for Mealtime Meal content (all food and drink) Nil 1/4 1/2 3/4 All Drinks (ml)
example, using a teaspoon for a yoghurt. Breakfast Bran flakes and sugar (2tsp), milk X 150ml
Coffee (no sugar)
16. After the meal ensure the patient is Mid morning 2 digestive biscuits X 150ml
clean and comfortable and has had enough
to eat and drink. Patients should be Coffee (no sugar)
encouraged to eat but should not be pres- Lunch Chicken pie, peas, potatoes, X 300ml
sured when they have indicated that they Chocolate sponge and custard X
have had enough. Glass of water x 2
Mid afternoon Cup of tea, slice of fruit cake X 150ml
17. Offer the patient a chance to clean their Evening meal Chicken salad sandwich, X 100ml
teeth and dentures or if this is not possible, strawberry mousse X
perform mouth care. Glass of milk
18. At the end of the meal ensure the Late evening/ Hot chocolate (no sugar) X 150ml
patient has a drink to hand but be aware overnight 1 digestive biscuit
that those who need help with eating will References
need help with drinking too and regular l Complaining of difficulty ea ting or Care Quality Commission (2015) The Fundamental
fluids should be offered. drinking; Standards. Bit.ly/FoodStandardsCQC
l R eluctance to eat certain consistencies; Council of Europe (2003) Ten Key Characteristics
19. Remove your apron, decontaminate l Feeling of food getting stuck in mouth, of Good Nutritional Care in Hospitals.
your hands and document the patient’s holding food in cheeks; Bit.ly/MealCharacteristics
dietary intake. l Food/drink falling out of the mouth. Department of Health (2014) The Hospital
Food Standards Panel’s report on standards
If you notice any of the above observe for food and drink in NHS Hospitals.
Documentation the patient for signs of aspiration pneu- Bit.ly/HospitalFoodStandards
Food and fluid charts are a vital way of monia; this occurs when patients have Dougherty L, Lister S (2015) The Royal Marsden
- - Hospital Manual of Clinical Nursing Procedures.
assessing patients’ nutritional status. Die swallowing problems and food inadvert Oxford: Wiley-Blackwell.
titians and nutrition teams rely on them ently enters the respiratory tract. Symp- Elia M (2015) The Cost of Malnutrition in England
- toms of aspiration pneumonia include: and Potential Cost Savings from Nutritional
when working out nutritional require Interventions. Bit.ly/MalnutritionCost
ments and the need for additional nutri- -
breathlessness, decreased oxygen satura Elia M, Russell CA (2009) Combatting
tion support. These charts are a useful tool tions tachycardia and pyrexia. If these are malnutrition: recommendations for action.
when assessing weight loss. An example of present, seek medical advice urgently. A report from the Advisory Group for Malnutrition.
a completed form is illustrated in Box 3. Bit.ly/CombatingMalnutrition
Reflection Leach RM et al (2013) Nutrition and fluid balance
Impaired swallow Look at your own area. Are patients pre- must be taken seriously. British Medical Journal;
346: 801.
Mealtime is an ideal opportunity to assess pared for meals? Do they have the help National Institute for Health and Care Excellence
swallowing. An urgent referral should be they need? Are all staff helping with (2006) Nutrition Support in Adults: Oral
made to a speech and language therapist if meals? If not, what are they doing? Can Nutrition Support, Enteral Tube Feeding and
the patient has any of the following symp- you make five small changes that will Parenteral Nutrition. Clinical Guidelines 32.
Bit.ly/NICENutrition2006
toms of dysphagia: improve the mealtime experience? National Patient Safety Agency (2011)
l Coughing/choking; Look at the food record charts – are they Dysphagia Diet Food Texture Descriptors.
l Wet/‘gurgly’ voice; completed accurately? If not, can you Bit.ly/FoodDescriptions
amb Nursing and Midwifery Council (2015a) The Code:
L l Taking a long time over a meal/ share good practice and ensure that all
Professional Standards of Practice and Behaviour
peter falling asleep; staff know how important it is? NT for Nurses and Midwives. Bit.ly/NMCCode2015
Nursing Times [online] November 2017 / Vol 113 Issue 11 25 www.nursingtimes.net
no reviews yet
Please Login to review.