181x Filetype PDF File size 0.23 MB Source: apjcn.nhri.org.tw
Asia Pac J Clin Nutr 2011;20 (2):161-168 161
Original Article
A simple meal plan of ‘eating vegetables before
carbohydrate’ was more effective for achieving glycemic
control than an exchange–based meal plan in Japanese
patients with type 2 diabetes
1 2 3 3
Saeko Imai PhD ,Mikuko Matsuda MA ,Goji Hasegawa MD ,Michiaki Fukui MD ,
4 5 2,3
Hiroshi Obayashi PhD , Neiko Ozasa MD , Shizuo Kajiyama MD
1Department of Clinical Nutrition, Faculty of Comprehensive Rehabilitation, Osaka Prefecture University,
Osaka, Japan
2Kajiyama Clinic, Kyoto, Japan
3Department of Endocrinology and Metabolism, Kyoto Prefectural University of Medicine, Graduate School
of Medical Science, Kyoto, Japan
4Institute of Bio-Response Informatics, Kyoto, Japan
5Department of Cardiovascular Medicine, Kyoto University, Graduate School of Medicine, Kyoto, Japan
This study aimed to determine whether educating diabetic patients to ‘eat vegetables before carbohydrate’ was as
effective on long-term glycemic control as a traditional exchange-based meal plan. To test this hypothesis, we
carried out a randomized, controlled trial in patients with type 2 diabetes that compared changes in HbA1c as the
primary outcome. A total of 101 patients were stratified according to sex, age, BMI, duration of diabetes, and
HbA1c, and then randomized to receive instructions to eat either vegetables before carbohydrate (VBC, n=69) or
an exchange-based meal plan (EXB, n=32). The impact of the two plans on glycemic control was compared over
24 months of follow-up. Significant improvements in HbA1c over 24 months were observed in both groups
(VBC, 8.3 to 6.8% vs EXB, 8.2 to 7.3%). HbA1c levels were significantly lower in the VBC group than in the
EXB group after 6, 9, 12 and 24 months of the study. Both groups exhibited similar improvements in dietary
practices with respect to intake of carbohydrate, fats and sweets, while the VBC group had a significant increase
in consumption of green vegetables and a significant decrease in fruit consumption. A simple meal plan of ‘eat-
ing vegetables before carbohydrate’ achieved better glycemic control than an exchange-based meal plan in Japa-
nese patients with type 2 diabetes over a 24-month period.
Key Words: type 2 diabetes, dietary interventions, glycemic control, vegetables, carbohydrate
INTRODUCTION between dietary constituents and glucose tolerance has
It is essential to manage good metabolic control in pa- contributed to the development of nutritional prescrip-
tients with diabetes in order to prevent chronic complica- tions, such as the food exchange system. Such strategies
1,2
tions. However, a significant number of patients with aim to restrict energy intake and provide macronutrient
diabetes remain poorly controlled, mainly as a result of balance. However, diabetic patients may have trouble
3-5
low compliance with eating a good diet. The important understanding diets based on a food exchange system,
choices that affect blood glucose control in people with and even if they do understand the system, they may have
3
diabetes are made by themselves, not by their physicians difficulty changing their daily food habits. In particular,
or other medical professionals. Patients need to make a elderly diabetic patients may experience difficulties im-
series of choices regarding eating and physical activity plementing the recommendations of the exchange-based
that are necessary to regulate blood glucose levels and meal plan.
prevent complications. It has been demonstrated that postprandial hypergly-
People with diabetes are advised to adopt an appropri- cemia is associated with increased risk for macrovascular
ate diet including dietary habits and meal patterns on a
lifelong basis. Frequently, the efforts of patients are not in
the appropriate direction, or alternatively they may re- Corresponding Author: Dr Saeko Imai, Osaka Prefecture Uni-
ceive confusing and contradictory advice from the media versity, 3-7-30, Habikino, Habikino, Osaka 583-8555, Japan.
or social contacts. Diabetes education, especially dietary Tel: 81-72-950-2111; Fax: 81-72-950-2127
education, requires training by medical professionals and Email: poooch@rehab.osakafu-u.ac.jp
provision of unequivocal information based on sound Manuscript received 27 April 2010. Initial review completed 8
evidence. Traditionally, recognition of the relationship November 2010. Revision accepted 9 March 2011.
162 S Imai, M Matsuda, G Hasegawa, M Fukui, H Obayashi, N Ozasa and S Kajiyama
disease.6 The recommendations of the International Dia- This study was a 2-year randomized controlled trial in
betes Federation in 2007 were intended to assist in devel- subjects with T2DM that compared the effectiveness and
oping strategies to effectively manage postprandial glu- acceptability of a simple meal plan that involved an inter-
cose levels in people with diabetes. Strategies for nutri- vention of eating vegetables before carbohydrate (VBC)
tional education should be re-organized to provide a sim- with a traditional exchange-based meal plan (EXB). The
ple and easy meal plan that lowers postprandial hypergly- primary outcome was changes in HbA1c, while secon-
cemia in patients with diabetes and has high compliance dary outcomes were changes in body weight, serum lipids,
on a lifelong basis. In a previous paper we reported an and blood pressure. Individual dietary counseling was
acute study of a simple meal plan that involved ‘eating provided by dietitians with the initial visit, including ex-
vegetables before carbohydrate’. We demonstrated a 20% tensive evaluation and education focused on self-care
reduction in postprandial plasma glucose and a 30% re- management. After the initial visit, patients were sched-
duction in postprandial serum insulin levels in patients uled for return clinic visits every month. The patients
7
with type 2 diabetes mellitus (T2DM). were also scheduled to see dietitians at every visit for 24
In addition to lowering acute postprandial glucose and months. The dietitians were trained in all aspects of in-
insulin responses, the current study aimed to determine struction and coping skills, which include menu planning
whether educating diabetic patients to ‘eat vegetables and making appropriate food choices. Instructions for the
before carbohydrate’ was as effective on long-term gly- VBC or EXB groups regarding diet and physical activity
cemic control as a traditional exchange-based meal plan. involved the same dietitian each time for each group.
To test this hypothesis, we carried out a randomized, con- Current dietary habits, physical activity and eating be-
trolled trial in patients with T2DM that compared changes havior were determined in all the participants prior to
in HbA1c as the primary outcome and changes in weight, intervention. Detailed written instructions for completion
serum lipids, and blood pressure as secondary outcomes. of the food diaries were provided and the participants
were encouraged to contact the dietitian if they had any
MATERIALS AND METHODS questions regarding this procedure. The dietary values
Participants were entered into a computer database and analyzed by a
The study was carried out between 2005 and 2009 at Ka- dietitian, using a dietary computer soft program (Eiyokun,
jiyama Clinic in Kyoto, specialized for diabetes treatment, Kenpakusya, Tokyo, Japan) based on Standard Tables of
8
using a protocol approved by the Ethics Committee of the Food Composition in Japan. Physical activity involving
School of Comprehensive Rehabilitation at Osaka Prefec- moderate exercise such as walking 30 to 40 min each day
ture University. We enrolled patients diagnosed with was recommended, and assessed in both groups using
T2DM who fulfilled the World Health Organization Kens Activity Monitor Life Corders® (Suzuken, Aichi,
(WHO) criteria for diabetes. Informed consent was ob- Japan) for 7 days prior to intervention and 21 days after
tained from all the subjects before enrollment in the study. intervention. Dietary restraint and overeating tendencies,
A total of 221 outpatients with T2DM from Kajiyama such as emotional and external eating were measured
9
Clinic were selected for possible participation in the study using the Dutch Eating Behaviour Questionnaire (DEBQ).
if they had no major complications or medical illnesses. The patients were required to complete the DEBQ at the
The exclusion criteria were as follows: (1) chronic liver initial visit and after 2 months of intervention. Emotional
disease or a clinical history and/or signs of cardiovascular eating was defined as eating in response to states of emo-
disease, cerebrovascular disease, or peripheral arterial tional arousal such as fear, anger or anxiety, while exter-
disease and (2) heavy smoking (more than 40 cigarettes a nal eating was classified as eating in response to external
day), and drinking (more than 50 g alcohol a day). A total food cues such as the sight and smell of food or eating in
of 148 patients were judged capable of performing basic response to food-related stimuli. Restrained eating was
self-management skills and able to participate in the study. defined as overeating after a period of slimming when the
Agreement to participate in the study was obtained from cognitive resolve to diet was abandoned.
101 patients, who were stratified according to sex, age,
2
body mass index (BMI; kg/m ), duration of diabetes, and Exchange-based meal plan (EXB) group
HbA1c. The patients were then randomized into two Patients in the EXB study group were instructed on both
groups to receive instructions on either a simple meal the food exchange system and portion size using educa-
plan that involved eating vegetables before carbohydrate tional material that consisted of “Food Exchange Lists:
(VBC group, n=69) without taking into account energy Dietary Guidance for Persons with Diabetes”which pro-
intake, or a traditional exchange-based meal plan (EXB vided a rough gauge on the amount of energy and nutri-
group, n=32) that used the food exchange system to focus ents contained in each food, as the basis for dietary in-
10
on energy intake. We set the number of participants in the structions. The exchange lists are used routinely as a
VBC group was be twice as much as the EXB group out method for meal planning in patients with diabetes. The
of ethical consideration for the participants. This is be- justification for specific food inclusions and general food
cause the VBC method is simple and easy to understand groups in the “Food Exchange Lists: Dietary Guidance
for the participants, and the VBC method was effective for Persons with Diabetes” is provided by a food database
for reducing postprandial plasma glucose and insulin lev- that includes associated energy and macronutrient val-
7 8
els as described previously. ues. The mean energy and macronutrient values for each
of the lists closely match the mean exchange values. The
Research design patients were recommended to consume more than 350g
of vegetables and 80 kcal of fruits a day. The intervention
Eating vegetables before carbohydrate 163
focused on setting individual and realistic goals in order pan), total cholesterol and triglyceride levels by an en-
to achieve gradual dietary change. Approximately 60 min zyme assay, high density lipoprotein (HDL) cholesterol
were spent on dietary counseling at the initial visit and 40 levels by a direct method (Labospect 008K, Bio Majesty
min at each subsequent session. Dietary intake was as- JCA-BM 8060, JEOL, Ltd, Tokyo, Japan), and low den-
sessed by food records collected over three days at the sity lipoprotein (LDL) cholesterol levels by an enzymatic
initial visit (baseline) and over seven days after 2 months method (Bio Majesty JCA-BM 8060, JEOL, Ltd, Tokyo,
of intervention. Japan).
Vegetables before carbohydrate (VBC) group Statistical analysis
The VBC method includes nutritional advice given in the All values are expressed as mean ± SD unless otherwise
form of a simple and easy meal plan of eating vegetables indicated. The measurements were analyzed using SPSS
first and carbohydrate last in each meal. In order to re- 15.0 for Windows (SPSS Inc, Chicago, IL, USA).
duce postprandial hyperglycemia, patients in the VBC Student’s t-test was used to test differences between the
group were encouraged to consume every meal eating two study groups and paired t-tests were performed to
vegetables prior to carbohydrate; green vegetables at least analyse within-group changes over time. Chi-square tests
once a day, not fruits, and chewing each bite more than were used to compare categorical data. Repeated-
20 times. Depending on the patient’s current dietary in- measures ANOVA was performed for comparisons
take, the intervention aimed to encourage increased con- among time (baseline and 12-month or 24-month of
sumption of vegetables, mushrooms, and seaweeds and follow-up) and the two study groups. Spearman’s
low glycemic index (GI) foods using an original educa- correlation coefficients were calculated to investigate the
tional brochure. The intervention focused on setting indi- association among dietary intakes and HbA1c, BMI, and
vidual and realistic goals in order to achieve gradual die- serum lipids levels. Differences were considered
tary change. Approximately 30 min were spent on dietary significant at p<0.05.
counseling at the initial visit and 20 min at each subse-
quent session. Dietary intake was assessed by food re- RESULTS
cords collected over three days at the initial visit (baseline) A flow diagram of the study with the number of patients
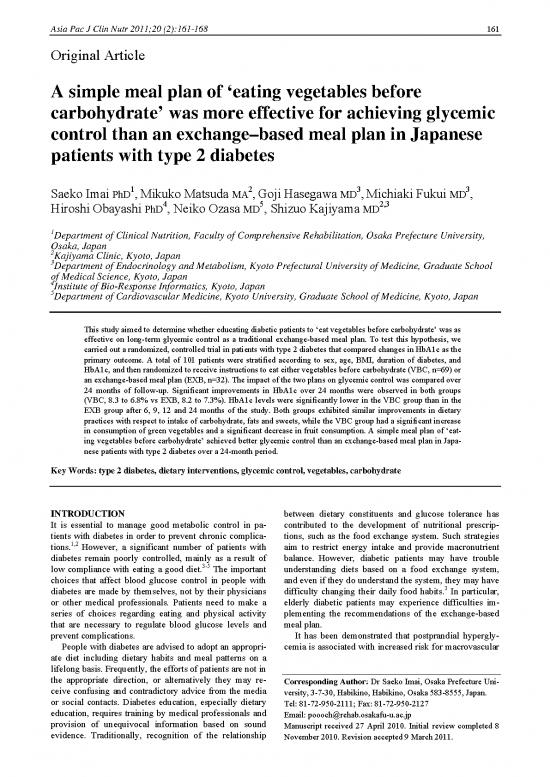
and over seven days after 2 months of intervention. is shown in Figure 1. Of the 69 participants who enrolled
in the VBC group, four patients (6%) dropped out from
Laboratory analyses the 2-year-study as a result of moving or changing medi-
Laboratory data, body weight and BMI measurements cal institutions, 65% of patients completed the dietary
were collected from all participants at baseline and every education over two years, and 4% took only one dietary
4 weeks thereafter for 24 months. Weight was measured session. In contrast, in the EXB group five participants
to the nearest 100 g without shoes while wearing minimal dropped out from the 2-year study (16%) out of 32 par-
clothes. Height was measured without shoes with the ticipants as a result of changing medical institutions, 31%
shoulders in the normal position. BMI was calculated as completed the dietary education over two years, and 28%
weight in kilograms divided by height in meters squared. took only one dietary session (p<0.001). The retention
Blood pressure was measured twice in the seated position rates of the study were 94% in the VBC and 84% in the
during the physical examination after the subject had EXB group at 24-month. The mean dietary sessions were
rested for 10 min. Fasting blood samples were collected 13.2±7.9 times in the VBC and 8.2±8.4 times in the EXB
from all the participants every 4 weeks in the morning (p<0.01) and dropouts rates were 33% in the VBC and
after an overnight fast. HbA1c levels (JDS: Japan Diabe- 69% in the EXB group in two years. Comparison of par-
tes Society) were determined by a latex cohesion method ticipants who withdrew from the sessions and the differ-
(JCA-BM2250, KYOWA MEDEX, Co, Ltd, Tokyo, Ja- ence of the mean dietary session between two groups over
the same period, showed participants in the VBC group
Outpatients with type 2
diabetes (n = 221) Excluded (n = 120)
Did not meet inclusion criteria (n = 73)
Refused to participate (n = 47)
Randomized
Accepted to participate
(n = 101)
Vegetables Before Carbohydrate (VBC) Exchanged Based Meal (EXB)
(n = 69) (n = 32)
Baseline (n=69) Baseline (n = 32)
12 mths (n = 68) 12 mths (n = 30)
24 mths (n = 65) 24 mths (n = 27)
Figure 1. Flow of participants through the study
164 S Imai, M Matsuda, G Hasegawa, M Fukui, H Obayashi, N Ozasa and S Kajiyama
Table 1. Characteristics of the patients at baseline in 8.8.8.888
two study groups
8.8.8.444
VBC EXB p
(n=69) (n=32) 8.8.8.000 ******
Gender (males / females) 31/38 17/15 0.443 )) ****
Age (yrs) 63.4±11.7 65.1±12.4 0.503 %% 7.7.7.666 **** **** **
2
BMI (kg/m ) 23.7±4.0 22.7±4.4 0.726 c (c ( **** ****
Duration of diabetes (yrs) 7.5±8.4 7.0±8.3 0.777 11 **** ****
SBP (mmHg) 132±15 136±25 0.391 HbAHbA 7.7.7.222 **** ****
DBP (mmHg) 75±11 77±13 0.651 ******
HbA1c (%) 8.3±1.7 8.2±1.8 0.642 ******
6.6.6.888
T-C (mg/dL) 213±34 220±32 0.377 ******†† ******†† ****** ****** ****** ******††††
HDL-C (mg/dL) 56±17 56±13 0.932 ******††
LDL-C (mg/dL) 129±30 138±28 0.166 6.6.6.444
000191919222333 666111212121111555828282222111444
TG (mg/dL) 141±87 144±83 0.866 mmonthsonths
Diabetes treatment
Diet only 21 9 0.504 Figure 2. Changes in mean HbA1c levels in patients in the VBC
OHA 39 19 0.480
group (closed diamond-shape) and EXB group (opened square)
OHA + insulin 9 4 0.607 over the 24-month follow-up period. Data are expressed as mean
(SE). Significant difference from baseline, *p<0.05, **p<0.01,
Data are means ± SD or n. † ††
SBP: systolic blood pressure, DBP: diastolic blood pressure, T- ***p<0.001. VBC group vs EXB group; p<0.05, p<0.01
C: total cholesterol, HDL-C: high density lipoprotein cholesterol,
LDL-C: low density lipoprotein cholesterol, TG: triglyceride, ids, and percentage of each therapy at baseline (Table 1).
OHA: oral hypoglycemic agents
As illustrated in Figure 2, HbA1c decreased significantly
soon after intervention and also over the 24-month fol-
were more likely to accept the dietary sessions and adapt low-up period in both groups. However, HbA1c levels
their eating habits. Using an ‘intention-to-treat’ model, were significantly lower in the VBC group compared to
analysis of fasting blood samples was performed for 68 the EXB group at 6, 9, 12 and 24 months after interven-
patients in the VBC group at 12 months and 65 patients at tion. Comparison of the two groups showed that patients
24 months. The corresponding values for the EXB group in the VBC group maintained better glycemic control
were 30 patients at 12 months and 27 patients at 24 after 6 months of intervention, with mean HbA1c being
months. less than 7.0% (Figure 2 and Table 2). Neither BMI, dia-
There were no significant differences between the stolic blood pressure nor serum lipids levels was signifi-
VBC and EXB groups for gender, mean age, duration of cantly different between the two groups at 12-month or
diabetes, HbA1c levels, BMI, blood pressure, serum lip- 24-month of follow-up (Table 2).
Table 2. Laboratory data after 12 and 24 months of follow-up in patients in the two study groups
Baseline 12-month 24-month p
1 1
time time × group
2
BMI (kg/m ) 0.963 0.320
VBC 23.7±4.0 23.3±4.8 23.6±3.8
EXB 22.7±4.4 23.7±4.4 22.7±4.3
SBP (mmHg) <0.001 0.381
*** † ***†
VBC 132±15 123±11 123±10
*
EXB 136±25 129±16 129±12
DBP (mmHg) <0.001 0.301
*** ***
VBC 76±11 70±8 69±8
*
EXB 77±13 72±10 71±8
HbA1c (%) <0.001 0.016
*** † *** † †
VBC 8.3±1.7 6.7±0.8 6.8±0.7
** *
EXB 8.2±1.8 7.2±1.1 7.3±1.1
TC (mg/dL) 0.004 0.180
***
VBC 213±34 197±31 205±35
* **
EXB 220±32 202±33 200±33
HDL-C (mg/dL) 0.315 0.459
VBC 56±17 58±16 58±16
EXB 56±13 54±14 57±14
LDL-C (mg/dL) <0.001 0.065
*** *
VBC 129±30 117±28 121±28
** ***
EXB 138±28 120±28 116±29
TG (mg/dL) 0.595 0.099
VBC 141±87 123±63 129±63
EXB 144±83 149±83 164±104
* ** *** † 1
Data are mean ± SD. p<0.05, p<0.01 , p<0.01 vs baseline. p<0.05 VBC vs EXB group, Repeated-measures ANOVA.
no reviews yet
Please Login to review.