229x Filetype PDF File size 0.86 MB Source: www.ncbi.nlm.nih.gov
Journal of the Royal Society of Medicine Volu'me 84 February 1991 69
Transdermal glyceryl trinitrate to
allow peripheral total parenteral nutrition:
a double-blind placebo controlled feasibility study
HTKhawaja MSFRCS' J D Williams MSC2 P C Weaver MDFRCS' 'Department ofSurgery,
St Mary's Hospital, Portsmouth P03 6AD and2Department ofMedical Statistics and Computing, Southampton
University, Southampton General Hospital, Southampton S09 4XY
Keywords: parenteral nutrition; peripheral infusion; glyceryl trinitrate
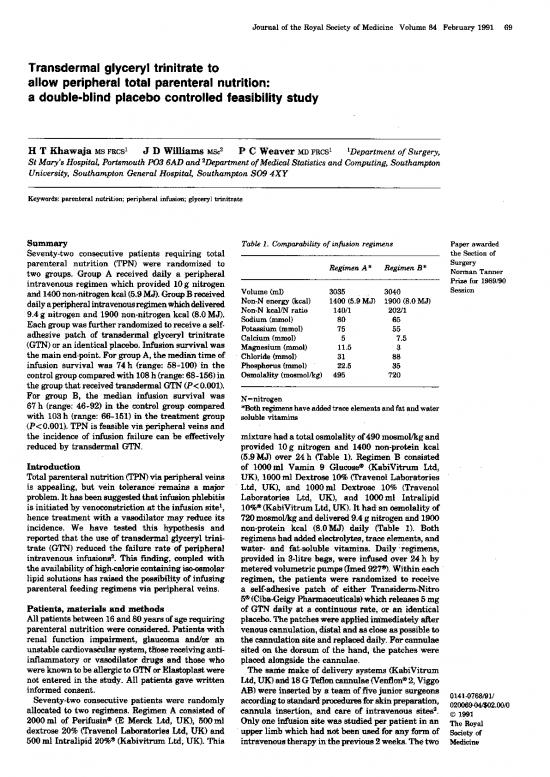
Summary Table 1. Comparability ofinfusion regimens Paper awarded
Seventy-two consecutive patients requiring total the Section of
parenteral nutrition (TPN) were randomized to Regimen A* Regimen B* Surgery
two groups. Group A received daily a peripheral Norman Tanner
intravenous regimen which provided 10g nitrogen Prize for 1989/90
and 1400non-nitrogen kcal(5.9MJ). GroupBreceived Volume (ml) 3035 3040 Session
dailyaperipheralintravenousregimenwhichdelivered Non-N energy (kcal) 1400 (5.9 MJ) 1900 (8.0 MJ)
9.4 g nitrogen and 1900 non-nitrogen kcal (8.0MJ). Non-N kcal/N ratio 140/1 202/1
Eachgroupwasfurtherrandomizedtoreceive a self- Sodium (mmol) 80 65
adhesive patch of transdermal glyceryl trinitrate Potassium (mmol) 75 55
(GTN)or an identical placebo. Infusion survival was Calcium (mmol) 5 7.5
the main end-point. For group A, the median time of Magnesium (mmol) 11.5 3
infusion survival was 74 h in the Chloride (mmol) 31 88
(range: 58-100) Phosphorus (mmol) 22.5 35
control group compared with 108h(range: 68-156) in Osmolality (mosmol/kg) 495 720
the group that received tranadermal GTN (P<0.001).
For group B, the median infusion survival was N=nitrogen
67 h (range: 46-92) in the control group compared *Bothregimenshaveaddedtraceelements andfatandwater
with 103 h (range: 66-151) in the treatment group soluble vitamins
(P<0.001). TPN is feasible via peripheral veins and
the incidence of infusion failure can be effectively mixture had atotal osmolality of490 mosmol/kg and
reduced by transdermal GTN. provided 10g nitrogen and 1400 non-protein kcal
Introduction (5.9MJ) over 24h (Table 1). Regimen B consisted
Total parenteral nutrition via of 1000 ml Vamin 9 Glucose (KabiVitrum Ltd,
is but vein (TPN) peripheral veins UK), 1000ml Dextrose 10% (Travenol Laboratories
appealing, tolerance- remains a major Ltd, UK), and 1000ml Dextrose 10% (Travenol
problem. It hasbeen suggestedthatinfusionphlebitis Laboratories Ltd, UK), and 1000ml Intralipid
is initiated by venoconstriction at the infusion site', 10%lo (KabiVitrum Ltd, UK). It had an osmolality of
hence treatment with a vasodilator may reduce its 720mosmollkg and delivered 9.4 g nitrogen and 1900
incidence. We have tested this hypothesis and non-protein kcal (8.0 MJ) daily (Table- 1). Both
reported that the use oftransdermal glyceryl trini- regimenshad added electrolytes, trace elements, and
trate (GTN) reduced the failure rate of peripheral water- and fat-soluble vitamins. Daily regimens,
intravenous infusions2. This finding, coupled with provided in 3-litre bags, were infused over 24 h by
the availability ofhigh-calorie containitng iso-osmolar meteredvolumetric pumps(lmied 9270). Within each
lipid solutions has raised the possibility of infusing regimen, the patients were randomized to receive
parenteral feeding regimens via peripheral veins. a self-adhesive patch of either Transiderm-Nitro
50(Ciba-Geigy Pharmaceuticals)whichreleases 5 mg
Patients, materials and methods of GTN daily at a continuous rate, or an identical
All patients between 16 and 80 years ofage requiring placebo. Thepatches were applied immediately after
parenteral nutrition were considered. Patients with venouscannulation, distal and as-close aspossible to
renal function impairment, glautoma and/or an the cannulation site and replaced daily. Forcannulae
unstable cardiovascular system, thosereceiving anti- sited on the dorsum of the hand, the patches were
inflammatory or vasodilator drugs -and those who placed alongside the cannulae.
wereknowntobeallergictoGTNorElastoplastwere The same-make of delivery systems (KabiVitrum
not entered in the study. All patients gave written Ltd, UK)and 18GTefloncannulae(Venflone2, Viggo
informed consent. AB)-were inserted by a team offivejunior surgeons 0141-0768/91/
Seventy-two consecutive patients were randomly according to standard procduresforskinpreparation, 020069-04/$02.00/0
allocated to two regimens. Regimen A consisted of cannula insertion, and care of intravenous sites2. © 1991
2000ml of Perifusin0 (E Merck Ltd, UK), 500ml Only one infusion site-was studied per patient in an The Royal
dextrose 20% (Travenol Laboratories Ltd, UK) and upper limb which had not been used for any form of Society of
500ml Intralipid 20%0 (Kabivitrum Ltd, UK). This intravenoustherapy intheprevious 2weeks. Thetwo Medicine
70 Journal of the Royal Society of Medicine Volume 84 February 1991
Table 2. Comparability ofgroups 100 ........................... lTet nt( = 8 ___Treatment (n = 18)
......... Control (n = 18)
-J 80 8
Regimen A Regimen B > 60
Control/lTreatment Control/Treatment
Age and sex distribution w
4 4
Median age (year) 59/59 60/59 20-.
(range) (38-71)/(35-72) (40-71)/(42-69) 20
Male 7/9 10/7 HOURS 0 20 40 60 80 100 120 140 160
Female 11/9 8/11
Site of cannulation Figure1. Relative survival ofinfusions in the treatment and
Dominant limb 2/3 1/2 control groups in infusion regimen A
Non-dominant 16/15 17/16
limb 100 -Treatment (n = 18)
Dorsum of hand 3/4 3/2 - .Control (n = 18)
Forearm 15/14 15/16 - 80
60 [
Table 3. Reasons for removal ofcannulae 4 40 [
A B -J 20
Regimen Regimen w
Control/Treatment Control/Treatment OL I
HOURS 0 20 40 60 80 100 120 140 160
Phlebitis 17/16 16/15 Figure2. Relative survival ofinfusions in the treatment and
Irregular drip rate 0/1 1/1 control groups in infusion regimen B
Extravasation 0/0 1/0
More than one 1/1 0/1
reason* phlebitis being the commonest cause of infusion
Accidental removal 0/0 0/1 failure (Table 3). The cannulation sites recovered
within 5 days in all patients, with the exception of
*Acombination ofphlebitis, extravasation and/or irregular one patient who had extravasation ofthe infusate. For
drip rate infusion regimen A, the median time of cannula
survival was 74 h (range: 58-100, n=18) in the control
infusion groups were studied simultaneously to avoid group compared with 108 h(range: 68-156, n=18) in
a possible time-related effect. the group that received Transiderm-Nitro 5® (Figure
The infusion was discontinued and the cannula 1; log rank x2=26.7, P<0.001). For infusion regimen
removed when it was no longerrequired fortreatment B, the median time of cannula survival was 67 h
or when it failed. Failure of infusion was defined as (range: 46-92, n=18) in the control group compared
the occurrence of phlebitis, extravasation or an with 103 h (range: 66-151, n=18) in the treatment
irregular drip rate. Phlebitis was defined as the group (Figure 2; log rank x2=32.5, P<0.001). This
presence oftwo or more ofthe following signs: pain, significantly increased cannula survival, associated
erythema, swelling, excessive warmth, or a palpable with the treatment group, is apparent for both
venous cord. infusion regimens. Combining the data from both
Venepuncture sites were inspected by the same regimens, we obtain estimated 96-h cannula sur-
investigator, together with a trained nurse, 12 hourly vival rate of 5.9% and 82.4% for the control and
or when an irregularity ofdrip rate or the patient's treatment groupsrespectively(difference=76.5%, 95%
discomfort were reported. Routine haematological and confidence interval (CI) for difference from 61.4%
biochemical monitoring for patients receiving TPN to 91.5%). A 95% CI for the proportion of cannulae
wascarried out in all cases. Data and adverse effects surviving in the treatment group at 96 h is 69.5%
were recorded on a standard form for each patient. to 95.2%. Comparison ofthecontrol groups in infusion
Incidence of infusion failure was analysed by life- regimens A and B showed that cannula survival
table methods. In particular, cannula survival was was greater in regimen A (log rank x2=4.7, df=1,
estimated using the method of Kaplan and Meier3 P=0.031). However, there was no significant differ-
andbetween group comparisons were made usingthe ence in cannula survival between the treatment
log rank test4. Cox's proportional hazard technique5 groups in both infusion regimens (log rank x2=0.3,
was used to assess the independent association of df=1, P=0.593).
treatment and regimen with cannula survival, Differences in infusion survival between control and
adjusting for confounding effects of age, sex, site of treatment groups, within each regimen, remained
cannulation and insertor. significant when allowance was made for differences
between the five doctors who inserted the cannulae,
Results age and sex ofpatients, and cannulae site using Cox's
The treatment and control groups in each infusion proportional hazard technique (relative risk offailure
regimen were comparable for age, sex, and site of in the treatment group=0.0039, 95% CI 0.0009 to
cannulation. The non-dominant limb was used more 0.0162). skin rash were the side effects
frequently than the dominant one with the forearm Headache and only
being the commonest site of cannulation (Table 2). noted and showed nobetween group difference (Table
Furthermore,therewerenosignificantbetween-group 4). One patient had a subcutaneous haematoma at the
differences in the reasons for removing the cannulae, site of cannulation, and venous cannulation, in two
Journal of the Royal Society of Medicine Volume 84 February 1991 71
Table 4. Adverse reactions incidence ofheadache in patients receiving TPN has
not been reported and it may be greater than in
Regimen A Regimen B the normal population. However, the incidence of
Control/Treatment Control/Treatnent headache in the treatment group (11.1% in regimen
A; 5.5% in regimen B) is not different from that
Headache 1/2 1/1 reported previously2'6. In all cases, the headache
Skin rash 1/0 0/0 responded to analgesia and the patients opted to carry
onwiththetrial. Onlyonepatientinthecontrolgroup
of regimen A had a skin rash which is, therefore,
likely to be due to the adhesive part of the patch.
Blackburn et al.16 advocated the use of isotonic
patients, was not achieved after two venepuncture aminoacids for peripheral intravenous feeding. Since
attempts. However, all three patients went on to have then, manyworkershaveinvestigatedthe metabolic
successful cannulation in the other upper limb. There effects of exogenous energy substrates, and have
was no clinical evidence ofcatheter sepsis, and none concluded that isotonic amino acids alone have no
ofthe patients had significant changes intheir blood significant protein-sparing effect'7"8 and that an
haematology andbiochemistry overthe studyperiod. ideal regimen should provide amino acids, fat and
glucose together with electrolytes, trace elements and
Discussion vitamins'8"9. However, the hypertonicity of such
The above results demonstrate the feasibility ofTPN mixtures has compelled clinicians to use central
via peripheral veins, and confirmthe previous reports rather than peripheral veins in order to avoid
that transdermal GTN reduces the incidence of peripheral venous phlebitis. Central venous cannu-
peripheral intravenous infusion failure26. lation requires skill and may be time consuming.
The aetiology of infusion phlebitis is multi- In our institution, we site all central venous feeding
factorial7. Duration and site of infusion, rate of lines under strict sterile conditions in the operating
flow, nature ofinfusate and drug additives including room. The complications of such technique are
the pH and particulate matter, size ofvein, cannula well documented20. Therefore, the use of paren-
size and material, trauma at venepuncture and teral feeding regimens employing a simpler, safer,
infection have all been incriminated. Several and cheaper method of venous access is appealing,
regimens have been suggested for prophylaxis buthas until recently not been considered practicable.
including in-line filtration, neutralization of acid There have been a few reports of peripheral
solutions and the addition ofsteroids and/or heparin intravenous administration ofTPNregimens. The use
to the infusate. However, these prophylactic measures of hyperosmolar solutions necessitated frequent
have their limitations and have not gained wide change of the infusion site due to phlebitis21.
approval. Addition of heparin (1 IU/ml), hydrocortisone (5 mg/
In clinical practice, hyperosmolar solutions and ml) or heparin (1 IU/ml) and hydrocortisone (5 mg/I),
irritant drugs are usually given via central rather and sodium hydroxide as a buffer (1.8 mEq/1) to
thanperipheral veinsbecause the greater blood flow the infusate resulted in improved vein tolerance22.
in central veins rapidly dilutes the infusate. Thus, the The reasons why these measures didn't gain wide
concept of increasing the blood flow in peripheral approval require further investigations. Furthermore,
veins is appealing and-may reduce the incidence of there is evidence that the addition ofheparin to the
infusion phlebitis. Transdermal GTN hasbeen shown infusate may result in creaming of lipid emulsions
to induce local vasodilatation8'9, and sublingual GTN due to the formation of calcium-heparin-lipid
has been reported to increase blood flow whilst complex23.
decreasing vascular resistance and venous tone inthe Thenon-protein calories intheregimensusedinthis
forearm'0. The drug has also been shown to stimu- study were relatively low. Elwyn?A and Macfie25
late synthesis of prostacyclin by cultured human haveshownthatestimations ofcalorierequirements
endothelial cells". Prostacyclin relaxes smooth have been excessive in the past and their work
muscle cells in vein walls and is also apotent inhibitor suggests that the energy inputs in our study are
of platelet aggregation. The maintenance of an adequate to meet the needs of many postoperative
effective concentration of prostacyclin at infusion patients. We did not carry out metabolic studies.
sites may prevent venoconstriction and platelet However, our patients remained clinically well and
aggregation; thereby possibly reducing the incidence biochemically stable throughout the study period.
of infusion phlebitis. Wilson et al.26 have reported good metabolic profiles
AnothercontributoryfactorenablingperipheralTPN in ±0 patients who were intravenously fed with a
maybetheuseoffatemulsions.Intralipid (KabiVitrum regimen similarto regimen A. Furthermore, it is now
Ltd, UK) contributed 71% and 58% of the non- well accepted that fat is a beneficial energy source.
nitrogen energy in regimens A and B respectively. We have recently reported good utilization of
It has been reported that the addition ofIntralipid® to intravenous lipid emulsions, when given as 50% of
a glucose solution buffers the vein wall and reduces non-nitrogen energy, with good intravascular
endothelial injury'2"3. Furthermore, a number of lipolysis, presumably due to activation of intra-
irritant drugs are now made up in lipid media, with vascular lipoprotein lipase27.
great improvement in vein tolerance (eg diazepam as The cannulae survived longer than 4 days in the
diazemuls®14, and etomidate15). majority ofpatients who received transdermal GTN,
Thepopulations inthetreatment andcontrol groups thus obviating the need for frequent changes of the
were comparable in terms of age, sex, and site of cannulation site. This fact, coupled with the early
cannulation. recovery ofthe infusion site, has relevance bothto the
The incidence of headaches and skin rashes were comfort of the patient and to the convenience of
similar in the control and treatment groups. The medical and nursing staff.
72 Journal of the Royal Society of Medicine Volume 84 February 1991
Wearenotadvocatingthatperipheral TPN should 7 Khawaja LIT. Infusion phlebitis (letter). Intensive Ther
replace central venous total parenteral nutrition Clin Monitoring 1988;9:190
in the hypercatabolic patients where the energy 8 Franks AG. Topical glyceryl trinitrate as adjunctive
requirements are great, or inthose patients requiring treatment in Raynaud's disease. Lancet 1982;i:76-7
parenteral nutritional support for a long time. 9 Hecker JF, Lewis GBH, Stanley H. Nitroglycerine
However, there are a number of patients in whom ointment as an aid to venepuncture. Lancet 1983;i:332-3
intravenous nutrition is indicated, butcentral venous 10 Mason DT, Braunwald E. The effects ofnitroglycerine
cannulation is not desirable. Such patients- include and amyl nitrite on arteriolar and venous tone in the
those who demonstrate signs of venous thrombosis, human forearm. Circulation 1965;32:755-66
those who need preservation of central lines for 11 Levin RI, Jaffe EA, Welzsler BB, Jack-Goldman K.
Nitroglycerine stimulates synthesis ofprostacyclin by
other clinical reasons, those with -complications cultured human endothelial cells. J Clin Invest 1981;
necessitating removal ofthe central line, and those 67:763-9 Reduction
who have commenced enteral feeding but in whom 12 FujiwaraT,Kawarasaki H,FonkalsrudEW.
the degree of absorption is not established. A ofpostinfusion venous endothelial injury with intralipid.
prospective survey in our hospital of248 consecutive Surg Gynecol Obstet 1984;158:57-65 Basaillon S.
patients who received central venous nutrition 13 Pineault M, Chessex P, Piedboeuf B,
showed that only 42 patients (17%) required feeding Beneficial effect ofcoinfusing a lipid emulsion on venous
for longer than 10 days(personal data). Therefore, we patency. JPEN 1989;13:637-40
now use peripheral nutrition as a holding regimen 14 Mattila MAK, Rossi ML, Ruoppi MK. Reduction of
pending reappraisal of nutritional needs. This venous sequelae of i.v. diazepam with a fat emulsion
as a solvent. Br J Anaesth 1981;53:1265-8
avoids complications ofcentral venous cannulation, 15 GranL,BleieH,JeppssonR,Maartmann-Moe. Etomidat
simplifies nursing care, reduces costs and may mit intralipid - ein losung zur schmerzfreien injection.
prevent delay in initiating nutritional support. Anaesthetist 1983;32:475-7
Furthermore, this route ofdelivery ofnutrients was 16 Blackburn GL, FlattJP, Clowes GHA, etal. Peripheral
widely accepted by the nursing staff and patients intravenous feeding with isotonic amino acid solutions.
alike. AmJSurg 1973;125:447-51
Webelievethatperipheral TPN is asafe alternative 17 Greenberg GR, Marliss EB, Anderson GH, etal. Protein
to central venous feedingformost patientsrequiring sparing therapy in postoperative patients. Effects of
short term intravenous nutrition and should be added hypocaloric glucose or lipid. N Engl J Med
considered when planning nutritional therapy. The 1976;294:1411-14 et al. Effect of
18 Khawaja HT, Jackson JM, Talbot ST,
use oftransdermal GTN makes such an alternative exogenous energy substrates on the metabolic response
feasible by improving vein tolerance. This technique to surgery (abstr.). Eur SurgRes 1986;18 (suppl 1): 1
ofperipheral intravenous feeding is certainly superior 19 Askanazi J, Carpentier YA, Elwyn DH. Influences of
to central venous TPN in terms of risks and total parenteral nutrition on fuel utilisttion in injury
complications. Whether or not it will prove meta- and sepsis. Ann Surg 1980;191:40-6
bolically adequate awaits further investigations. 20 Mughal MM. Complications of intravenous feeding
catheters. Br J Surg 1989;76:15-21
Acknowledgment: Wethankthenursingstaffofthegeneral 21 FraserI, Slater N, Howard P, etal. Peripheral parenteral
surgical wards at St Mary's Hospital for their cooperation, 22 nutrition. Br J Parenteral Ther 1986;7:144-8 R. Pre-
MrMRThompson, Consultant Surgeon, and Dr M Ford of Makarewicz PA, Freemen JB, Fairfull-Smith
Ciba Geigy UK for supply ofTransiderm-Nitro 5®/placebo vention of superficial phlebitis during peripheral
patches. parenteral nutrition. Am J Surg 1986;151:126-9
23 Rattenbury JM, Timmins JG, Cawthorne EA, et al.
References Identification of the cause of separation (creaming) of
lipid emulsions in intravenous infusion. J Pediatr
1 Hecker JF, Fisk GC, Lewis GBH. Phlebitis and extra- Gastroenterol Nutr 1989;8:491-95
vasation ("tissuing") with intravenous infusions. Med J 24 ElwynDH,KinneyJM,AskanaziJ. Energyexpenditure
Aust 1984;140:658-60 in surgical patients. Surg Clin North Am 1981;61:545-56
2 Khawaja HT, Campbell MJ, Weaver PC. Effect of 25 MacFie J. Active metabolic expenditure of gastro-
transdermal glyceryl trinitrate on the survival of peri- intestinal surgical patients receiving intravenous
pheral intravenous infusions: a double-blind prospective nutrition. JEPN 1984;8:371-6
clinical study. Br J Surg 1988;75:1212-15 26 WilsonA, GoodeAW, KirkCJC, SugdenM. Parenteral
3 Kaplan EL, Meier P. Non-parametric estimation for nutrition via peripheral veins: a feasibility study. JR
incomplete observations. JAm StatAssoc 1958,53:475-81 Soc Med 1987;80.430-3
4 Peto R, Pike MC, Armitage P. Design and analysis of 27 JacksonJM, KhawajaHT,TalbotST,LeeHA.Theeffect
randomizedclinical trials requiringprolonged observation ofsurgery andnutritional regimen onplasma lipoproteins
ofeach patient. (ii). Analysis and examples. Br JCancer and fat metabolites in man. Clin Nutr 1990;9:1-7
1977;35:1-39
5 Cox DR. Regression models and life tables (with NB:Furtherreferencescanbeobtainedfromtheauthor
discussion). J R Stat Soc B 1972;34:187-220
6 Wright A, Hecker JF, Lewis GBH. Use oftransdermal (Accepted31 July1990. Correspondence to MrHTKhawqaa,
glyceryl trinitrate to reduce failure of intravenous Department ofSurgery, King's College School ofMedicine
infusion due to phlebitis and extravasation. Lancet and Dentistry, Rayne Institute, 123 Coldharbour Lane,
1985;ii:1148-50 London SE5 9NU)
no reviews yet
Please Login to review.