138x Filetype PDF File size 0.27 MB Source: www.papsy.org
10/27/2017
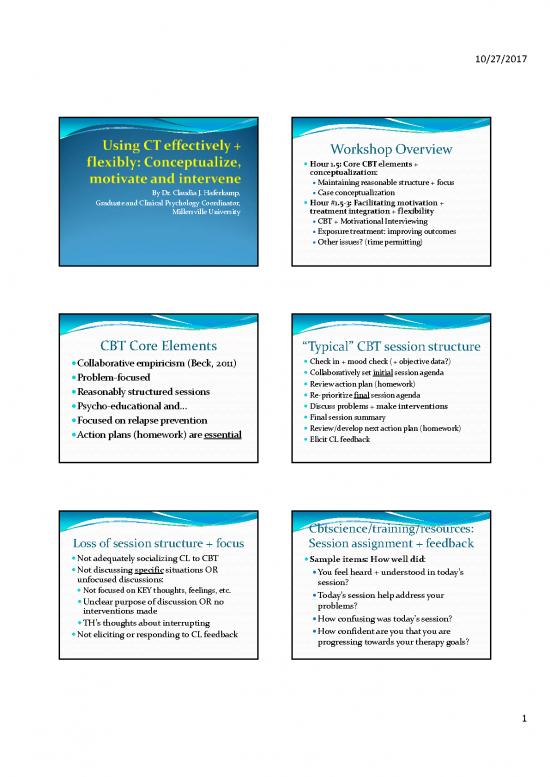
Workshop Overview
Hour 1.5: Core CBT elements +
conceptualization:
Maintaining reasonable structure + focus
By Dr. Claudia J. Haferkamp, Case conceptualization
Graduate and Clinical Psychology Coordinator, Hour #1.5‐3: Facilitating motivation +
Millersville University treatment integration + flexibility
CBT + Motivational Interviewing
Exposure treatment: improving outcomes
Other issues? (time permitting)
CBT Core Elements “Typical” CBT session structure
Collaborative empiricism (Beck, 2011) Check in + mood check (+ objective data?)
Problem‐focused Collaboratively set initial session agenda
Reasonably structured sessions Review action plan (homework)
Re‐prioritize final session agenda
Psycho‐educational and… Discuss problems + make interventions
Focused on relapse prevention Final session summary
Action plans (homework) are essential Review/develop next action plan (homework)
Elicit CL feedback
Cbtscience/training/resources:
Loss of session structure + focus Session assignment + feedback
Not adequately socializing CL to CBT Sample items: How well did:
Not discussing specificsituations OR You feel heard + understood in today’s
unfocused discussions: session?
Not focused on KEY thoughts, feelings, etc. Today’s session help address your
Unclear purpose of discussion OR no problems?
interventions made How confusing was today’s session?
TH’s thoughts about interrupting
Not eliciting or responding to CL feedback How confident are you that you are
progressing towards your therapy goals?
1
10/27/2017
Why form working hypotheses?
CBT Conceptualization (Persons, 2015)
Can’t treat what you can’t conceptualize One causal mechanism may underlie
Conceptualizations help us: multiple problems
Organize CL info ESTs may target a singledisorder ONLY
Develop working hypotheses There are no ESTs for many disorders
Develop treatment plans + rationales for Helps us address therapy‐interfering
interventions thoughts + behaviors
Build the working alliance
Persons: Case Formulation Case formulation example (adapted)
(Ledley et al., 2010)
Inclusive problem list Mike’s parents held him to exacting standards and sent
Origins him to schools known for academic rigor (ORIGINS).
Precipitants (large events trigger current episode) As a result, Mike started seeing others as critical and
feared being rejected for making mistakes (CAUSAL
Antecedents (activating situations): triggers MECHANISMS). These thoughts occurred after
symptoms deciding to enter the priesthood (PRECIPITANT).
Behaviors Afterwards he had ATs such as, “I make more mistakes
Consequences (functional) than others” and “people will notice my
anxiety…they’ll think I’m incompetent” resulting in
Causal mechanisms (mostly cognitive) increased (social) anxiety (i.e., blushing, sweating,
Organismic variables (unique vulnerabilities) sleep disruption) (SYMPTOMS/PROBLEMS).
Case formulation (cont.) Inclusive problem lists
Having to give his first sermon triggered his anxiety Problem areas: Problems with lists:
again (ACTIVATING SITUATION). Mike coped by Health, psychiatric Using vague terms/traits:
over‐preparing sermons, only spoke to familiar people Interpersonal/family Why is it a problem?
at social events and avoided discussing the priesthood Ignoring non‐
with his family (MECHANISMS). This temporarily Job/school psychological problems
reduced his anxiety (FUNCTIONAL Financial CL has “solved” it (?)
CONSEQUENCES) but he missed making valuable Housing DO: describe symptoms
social contacts and did not self‐disclose with his Legal DO: look for themes or
mentors which left him feeling more dejected and relationships among
unsure of his future (SYMPTOMS/PROBLEMS). Leisure functioning problems
2
10/27/2017
What should be on Mike’s David Tolin (Doing CBT, 2016)
problem list? Automatic + Semi‐Automatic cognition
#1: Automatic thoughts > trigger mood congruent
#2: attention + recall
#3: Intermediate beliefs (Semi‐Automatic)
Cognitive distortions, rules, interpretations
#4: Core beliefs/schemas (Semi‐Automatic) > may
#5: trigger compensatory strategies (Young et al., 2006):
Maintenance/Surrender (do the usual…)
Avoidance/Escape (avoid your triggers)
Compensation/Counter‐Attack (do the opposite)
AT: (Automatic)
Activating sit.: They’ll see memory
Mike asked to me sweat or bias: Recalls Why behavior is so important
deliver his first make other social
sermon mistakes in anxieties, World responds to what we say/do, not what
the sermon mistakes
Consequences: high we think
anxiety, blushing, Guideline #1: Do better in order to feel better
sweating, “rough” Origins: critical
performance parents; Guideline #2: Do the healthyopposite:
demanding
schools Teaches new coping skills
Compensatory (Semi‐ Disconfirms one’s (maladaptive) beliefs
Responses: (Semi‐ Automatic
avoids eye automatic) ) CB: I’m a Guideline #3: Avoid avoidance:
contact; looks Interpretation: loser who
down; talks fast It’s hopeless. messes up
(to finish I’ll always Short‐term gain may enable long(er) term pain
sermon sooner) screw up
cbtscience/training/resources:
ESTs: Lack of response Lack of progress worksheet
40% of CLs are in Pre‐Contemplation stage Sample “lack of progress” factors:
(Prochaska et al., 2014) Relationship is weak, problematic
Driessen et al., 2013: 16 sessions of CBT vs. Little is known about treating CL’s disorder
psychodynamic therapy: Goals are unrealistic (or we disagree on them)
No differences on any outcome measures Treatment dose is not meeting CL’s needs OR
Average 22% remission CL needs adjunct (or different) treatment
Friborg & Johnsen (2017): results of CBT for My own/CL’s behaviors are interfering w/treatment
unipolar depression declined over time Substance use is interfering with treatment
CL has high social strain or lacks social supports
3
10/27/2017
David Burns:
Outcome + Process Resistance Beck: Therapy interfering beliefs
Outcome:CL resists due to “magical thinking,” If I try + solve problems >>>
i.e., superstitious beliefs about treatment I’ll fail OR have to become more responsible
outcomes: It means my TH is controlling me + I’m weak
My anxiety protects me from something worse If I get better, my life will get worse. WHY?
My depression is the price I must pay for my sins CL fears not meeting others’ (new) expectations
Process:CL resists interventions due to magical Loss of social support or enabling relationships
thinking: Facing life challenges directly: may lose your
Exposure treatment resistance: My anxiety disability, lose your therapist, etc.
protects me from X
Other treatment challenges Integrating CBT + MI for anxiety
(Ledley, et al., 2010) (Randall & McNeil, 2016
CL thinkss/he must discuss the past in order to CBT elements consistent with MI:
get better Problem‐oriented > clear change targets
CL thinks her/his problems are biologically Highly collaborative relationship
determined Case formulation used to guide active
CL thinks that CBT may not work for her/him treatment planning
Are CL’s meds interfering with treatment? Focus on skills + behavior change
CL’s attributions for change when taking
meds?
Enhancing Motivation: Enhancing Motivation:
Key MI processes Key MI processes
Engaging: Solid relational foundation Evoking: Draw out CL’s reasons for change:
Accurate empathy Listen for “change talk” (vs. sustain talk)
OARS to understand ambivalence Selectively reinforce + summarize change talk
Avoid the “righting” reflex (expert trap) Elicit‐Provide‐Elicit
Focusing: Guide CL to a key change target: Planning: Bridge to change:
Identify behavior about which CL feels Selectively reinforce commitment language
ambivalent Determine readiness for change + assist with
What’s important to you? What could get in the specific change plans
way?
4
no reviews yet
Please Login to review.