237x Filetype PDF File size 0.44 MB Source: www.health.qld.gov.au
.au
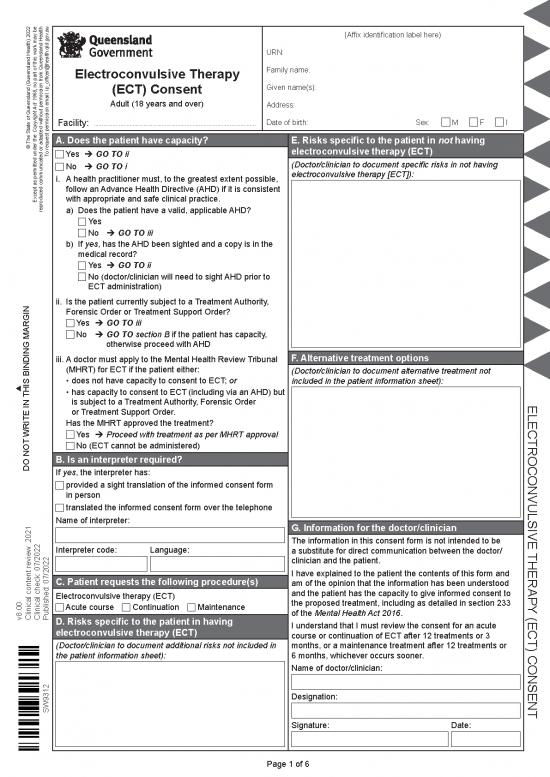
(Affix identification label here)
URN:
Electroconvulsive Therapy Family name:
, no part of this work may be (ECT) Consent Given name(s):
1968 Adult (18 years and over) Address:
Facility: ......................................................................................................... Date of birth: Sex: M F I
Copyright Act
The State of Queensland (Queensland Health) 2022A. Does the patient have capacity? E. Risks specific to the patient in not having
© o request permission email: ip_officer@health.qld.gov electroconvulsive therapy (ECT)
T Yes è GO TO ii
No è GO TO i (Doctor/clinician to document specific risks in not having
i. A health practitioner must, to the greatest extent possible, electroconvulsive therapy [ECT]):
follow an Advance Health Directive (AHD) if it is consistent
Except as permitted under the reproduced communicated or adapted without permission from Queensland Healthwith appropriate and safe clinical practice.
a) Does the patient have a valid, applicable AHD?
Yes
No è GO TO iii
b) If yes, has the AHD been sighted and a copy is in the
medical record?
Yes è GO TO ii
No (doctor/clinician will need to sight AHD prior to
ECT administration)
ii. Is the patient currently subject to a Treatment Authority,
Forensic Order or Treatment Support Order?
Yes è GO TO iii
No è GO T O section B if the patient has capacity,
otherwise proceed with AHD
iii. A doctor must apply to the Mental Health Review Tribunal F. Alternative treatment options
(MHRT) for ECT if the patient either: (Doctor/clinician to document alternative treatment not
• does not have capacity to consent to ECT; or included in the patient information sheet):
THIS BINDING MARGIN • has capacity to consent to ECT (including via an AHD) but
is subject to a Treatment Authority, Forensic Order ELECTROCONVULSIVE
or Treatment Support Order.
Has the MHRT approved the treatment?
WRITE IN Yes è Proceed with treatment as per MHR T approval
No (ECT cannot be administered)
B. Is an interpreter required?
DO NOT If yes, the interpreter has:
provided a sight translation of the informed consent form
in person
translated the informed consent form over the telephone
Name of interpreter: G. Information for the doctor/clinician
The information in this consent form is not intended to be
Interpreter code: Language: a substitute for direct communication between the doctor/ THERAPY
clinician and the patient.
C. Patient requests the following procedure(s) I have explained to the patient the contents of this form and
am of the opinion that the information has been understood
Electroconvulsive therapy (ECT) and the patient has the capacity to give informed consent to
Acute course Continuation Maintenance the proposed treatment, including as detailed in section 233 (ECT) CONSENT
v8.00Clinical content review: 2021Clinical check: 07/2022Published: 07/2022D. Risks specific to the patient in having of the Mental Health Act 2016.
electroconvulsive therapy (ECT) I understand that I must review the consent for an acute
course or continuation of ECT after 12 treatments or 3
(Doctor/clinician to document additional risks not included in months, or a maintenance treatment after 12 treatments or
the patient information sheet): 6 months, whichever occurs sooner.
Name of doctor/clinician:
SW9312 Designation:
Signature: Date:
Page 1 of 6
.au
(Affix identification label here)
URN:
Electroconvulsive Therapy Family name:
(ECT) Consent Given name(s): , no part of this work may be
Adult (18 years and over) Address: 1968
Date of birth: Sex: M F I
Copyright Act
H. Patient consent The State of Queensland (Queensland Health) 2022
I acknowledge that the doctor/clinician has explained: © o request permission email: ip_officer@health.qld.gov
T
• the “Electroconvulsive therapy (ECT)” patient information
sheet
• the medical condition and proposed treatment, including the
possibility of additional treatment Except as permitted under the
• the specific risks and benefits of the procedure reproduced communicated or adapted without permission from Queensland Health
• the prognosis, and risks of not having the procedure
• alternative treatment options
• that there is no guarantee the procedure will improve the
medical condition
• that if a life-threatening event occurs during the procedure, I
will be treated based on documented discussions (e.g. AHD
or ARP [Acute Resuscitation Plan])
• that a doctor/clinician other than the consultant/specialist
may assist with/conduct the clinically appropriate treatment;
this may include a doctor/clinician undergoing further training
under supervision
• that if the doctor/clinician wishes to record video, audio or
images during the procedure where the recording is not
required as part of the treatment (e.g. for training or research
purposes), I will be asked to sign a separate consent form.
If I choose not to consent, it will not adversely affect my
access, outcome or rights to medical treatment in any way.
I give my consent freely and voluntarily. THIS BINDING MARGIN
I was able to ask questions and raise concerns with the
doctor/clinician.
I understand I have the right to change my mind regarding
consent at any time, including after signing this form (this WRITE IN
should be in consultation with the doctor/clinician).
I have received the following consent and patient DO NOT
information sheet(s):
“Electroconvulsive therapy (ECT)”
“General anaesthetic”
On the basis of the above statements,
I consent to having electroconvulsive therapy (ECT).
Name of patient:
Signature: Date:
Page 2 of 6
.au
Electroconvulsive therapy (ECT)
Adult (18 years and over) | Informed consent: patient information
, no part of this work may be
1968
A copy of this form should be given to the patient to read carefully and allow time to ask any
questions about the procedure. The consent form and patient information sheet should be
Copyright Act included in the patient’s medical record.
The State of Queensland (Queensland Health) 2022
© o request permission email: ip_officer@health.qld.gov
T 1. What is electroconvulsive therapy (ECT) and how will it help
me/the patient?
Except as permitted under the reproduced communicated or adapted without permission from Queensland HealthElectroconvulsive therapy (ECT) has been used across the world as an effective treatment
for some severe mental illnesses for many years.
The value of this treatment is known internationally and the method has been improved in
recent years to get better results and fewer side effects. Modern ECT is safe for most people
(exceptions are now rare) and for some conditions, ECT is the best and safest treatment
option. ECT will not be given to anybody deemed unfit for treatment and your physical health
such as a cardiac condition will be assessed as a part of this. ECT is not painful.
ECT is good for major depression, mania and some forms of schizophrenia. In depression, it
is particularly good for those people who are very depressed and those who may be suicidal.
It is used in the treatment of depression when antidepressants have not worked. It is also
used for patients who have bad side effects with antidepressants or whose medical condition
means they can’t take antidepressants safely.
THIS BINDING MARGINYour doctor/clinician will discuss with you why ECT is the best treatment for you and what
other relevant treatment options are available.
ECT can help you by treating your condition which may also help you in the lifting of
WRITE IN depression and better thinking ability.
Duration of treatment
DO NOT
Acute course or continuation of ECT treatment sessions, usually given 1 to 3 times per week.
This consent is current for up to 3 months or 12 treatments, whichever is sooner. After that time
the doctor/clinician will review my consent with me if further treatment is to be given. When
significant changes occur in treatment, consent must be sought again and a new form signed.
Maintenance (preventative treatment given at intervals between weekly and monthly) course
of ECT treatment sessions for up to 12 treatments or 6 months, whichever is sooner. After that
time the doctor/clinician will review my consent with me if further treatment is to be given. When
significant changes occur in treatment, consent must be sought again and a new form signed.
Preparing for the treatment
Before your treatment, you will need to have some tests including an ECG, chest x-rays,
a physical examination, and a blood test(s).
Your doctor/clinician will explain these tests and when to have them.
• You must fast (eat no food or drink any fluid or water) for several hours before the ECT
treatment to ensure your stomach is empty
• If you do eat or drink anything within the fasting period, you must tell the nursing or medical
staff and your treatment may be reassessed or rescheduled
Electroconvulsive therapy (ECT) patient information
SW9312 v8.00 Clinical content review: 2021 Clinical check: 07/2022 Published: 07/2022 Page 3 of 6
• You MUST tell the doctor/clinician if there is During the treatment, the anaesthetist will
any chance you may be pregnant. continue to give you oxygen via a mask and
Your doctor/clinician may have to change the monitor your heart rate and oxygen level.
medication you were taking before ECT, as You will be asleep during all of this treatment,
some medications can affect how well the which means that you will not feel or
ECT works. remember any of the actual treatment.
On the morning of the treatment day, some Within a few minutes, the anaesthetic
medication will still be given but with a tiny medication will have worn off and you will
sip of water. wake up. During this time, you will be moved
During the procedure to the recovery room where you will be
monitored until you are awake enough to
You will be brought into the treatment area return to your ward (or wait to be taken home
and asked to lie down on a trolley. Staff will if you are having day procedure ECT).
attach some medical equipment to you:
• a blood pressure cuff on your arm 2. What are the risks?
• a small device over a finger to check pulse
and oxygen levels in your blood Modern ECT and general anaesthetic
• small stick-on electrodes are placed on treatment is usually completed in a short
your forehead and behind your ears to period of time and serious complications are
record the brain’s electrical activity during uncommon.
the treatment There are risks and complications with this
• extra equipment may be used if there are procedure. There may also be risks specific
extra risk factors that are known from your to each person’s individual condition and
medical history, examination or tests circumstances. Please discuss these with the
• a facemask is placed over your nose and doctor/clinician and ensure they are written
mouth to give you oxygen; this is to prepare on the consent form before you sign it. Risks
your body and brain for the extra activity include but are not limited to the following:
that will happen briefly with the treatment.
You will have a short general anaesthetic so Common risks and complications
you will be asleep and not feel or remember • immediately after ECT most people have
the treatment. The anaesthetic medication a short period of confusion and do not
will be injected into a vein, to make it work remember the actual treatment
quickly. • short-term memory may be affected
• existing memory problems, caused by your
A special anaesthetic doctor (anaesthetist) illness, may also get worse
will give the anaesthetic. You will also be • memories of events from your past are
given a muscle relaxant to keep any muscle less likely to be affected than short-term
reaction to the ECT at a safe level. memories
A doctor/clinician who has specialised • although specific memories may not return,
training in ECT gives the treatment in a overall memory will usually get better in the
special ECT treatment area. The doctor/ weeks to months after treatment
clinician puts the treating electrodes to your • anaesthetic side effects, such as headache,
scalp and passes a measured amount of nausea, vomiting; if these occur, tell the
electricity to a part of the brain to cause a staff looking after you, who will be able to
seizure (fit). The seizure will last about give you some medication to help
1 minute. This should not be confused with • muscle soreness due to either the muscle
the electrical stimulation which is brief and relaxants or the muscle activity caused by
lasts only for a few seconds. the seizure
• a temporary rise in blood pressure and
heart rate followed by a slowing of the
heart rate.
Electroconvulsive therapy (ECT) patient information
SW9312 v8.00 Clinical content review: 2021 Clinical check: 07/2022 Published: 07/2022 Page 4 of 6
no reviews yet
Please Login to review.